Collaborative care and Health IT.
In the ever-evolving world of health care, a figure whose role was once greatly limited in scope is beginning to take center-stage in the diagnosis process. Previously, the patient was treated more like a bottom-tier employee, expected to blindly obey orders handed down by minds deemed more expertly versed in specialized disciplines. Now, there are quite a few healthcare-related websites, like WebMD, Symptom checker, and Google, that provide patients with a means of becoming more conversant with medical methodology and terminology. The latest buzzword, though, is interoperability. Due to the abundance of healthcare websites and all the available data, there has to be a way to manage and streamline the information. Patient safety, patient care, and cost-effective healthcare will benefit from this collaborative effort and should be the driving factor.

Photo by Carlos Muza on Unsplash
More importantly, such healthcare websites serve as indicators supporting the proposal that patients should be more involved; have more say in their medical treatment. Typical “patient/physician” interaction and key studies show that patients are, in fact, taking more active roles in their care. Patients realize that inserting an “I” into the “team” of physicians tasked with maintaining their health makes sense. Increasing numbers of doctors are coming to similar conclusions. Understanding “Collaborative Care,” as a shift in the medical diagnosis process, leads to a demand made by physicians to establish more efficient lines of communication and provide more reliable resources.
“Collaborative Care” is simply a term, like “Integrated Care” or “Shared Care,” that, while used to define a range of varying philosophies on medical treatment, is based upon the notion that patient care is becoming increasingly team-oriented. Dove Press Patient Intelligence Journal conducted a study, asking patients: “Have you ever asked your physician to prescribe something different than the original recommendation?” 34% responded: yes. More telling was the fact that 69% percent of doctors agreed to prescribe the alternate medication. Patients are playing a larger role in their treatment because they are more informed. An article by John Mooney, co-founder of “collaborativeCARE Conference,” asserts that the “informed patient” is the primary reason that health care treatment needs to adapt, becoming more “inclusive, integrated, and collaborative.” Shifting the backbone of health care delivery to accommodate patients’ increasingly relevant roles is an inarguable necessity.
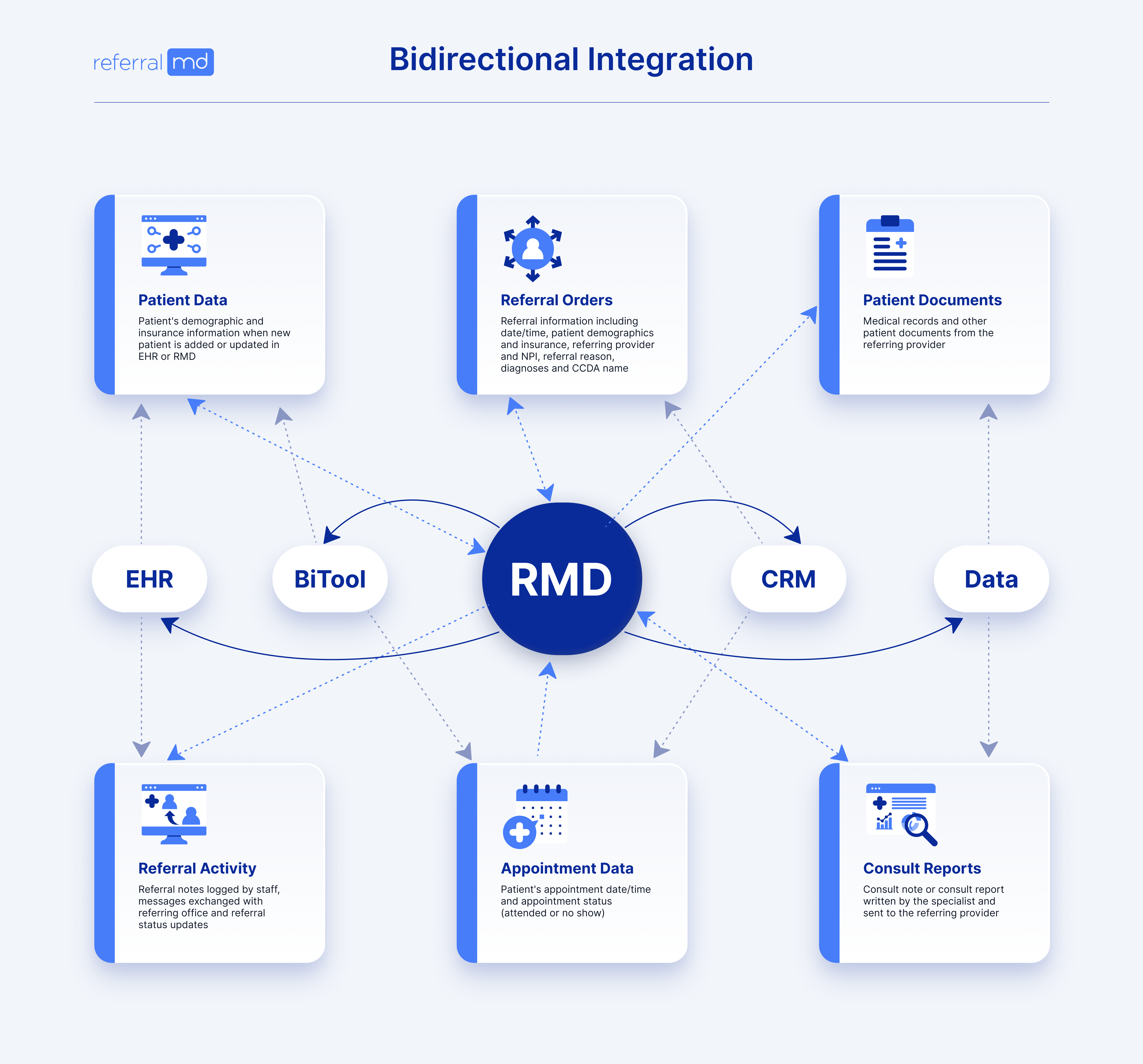
Establishing a more collaborative approach to patient care can mean several things, but all are based upon making changes that facilitate better communication. Specialists must work more closely with primary physicians while providing patients with access to medical knowledge more reliable than a hastily written posting found on an online medical bulletin board. Making communication between primary caregivers and specialists easier involves ensuring that patient records can be shared quickly with an electronic referral management application as ReferralMD provides, with updates to patient files occurring just as quickly.
Such simplification, allowing physicians to communicate more effectively, would greatly reduce patient file errors. This, in turn, would establish a more dependable knowledge base for physicians, allowing them to inform and guide their patients more effectively. Patients have access to a wealth of global medical knowledge. Still, such information should act as a supplement, not a substitute, for the personalized guidance provided to them by their primary doctor.
As healthcare, IT needs to evolve, and new demands are made. Changes in how patient care is approached become more defined by a need to stay up-to-date with technology and the fervid rate at which medical information is disseminated. These notable factors have cultivated a health care culture that must adapt to serve a more knowledgeable patient base, whose increased accountability and interest in their health have led to doctors’ need to modify their own roles.
A focus on pushing for a more integrated approach to health care is vital in moving towards more effective patient-oriented treatment. This push cannot happen without making strides to ensure doctors are better equipped to handle patient needs. Communication between physicians must become more proficient. Only then can it be assured that patients receive the best level of guidance from a network of physicians working in collaboration to inform their decisions best. The “informed patient” is an integral part of the diagnosis team, and playing on a team means making sure everyone is on the same page, and everyone has a playbook they can rely upon.
What do you think can be done better to improve communication between providers? Tell us your story.
Works Cited
“Collaborative Care.” Wikipedia, the Free Encyclopedia. Web. 05 Oct. 2011. <http://en.wikipedia.org/wiki/Collaborative_Care>.
Mooney, John. “Why the Time Is Right for Collaborative Care.” KevinMD.com | Social Media’s Leading Physician Voice. Web. 05 Oct. 2011. <http://www.kevinmd.com/blog/2011/02/time- collaborative-care.html>.