Healthcare systems around the world are continuously evolving. Personalized medicine, popularly known as precision medicine, is one such approach that different healthcare systems around the world are trying to incorporate into their current medical practice as much as they can.
Precision medicine, as the name suggests, intends to deliver precise and individualized treatment to patients based on their genetic understanding of their disease or condition. It is an approach that lets doctors choose a treatment plan for patients that is most likely to suit them as per their disease characteristics.

Precision medicine is not a new concept. It has always been there in practice in case of specialized and critical procedures. For example, it follows the principles of organ transplantation. Before an organ transplant surgery, several tests are conducted to check the compatibility to eliminate the chance of organ rejection.
Additionally, the patient is made to undergo a series of tests to study his individual organ failure characteristics such as genetic history, blood profile, allergies to specific drugs, and functioning of the other organs. All of this information is used to choose the right donor and administer the treatment that is most likely to suit the individual needs of the patients. Precision medicine works in the same manner with a difference that it has a greater focus on the genetic understanding of the disease that the patient is suffering from.
Precision medicine is most likely to play a great role in cancer treatment. Until now, all cancer patients who are diagnosed with a similar form of cancer, stage, and grade are treated using the same approach. Despite similar treatment, doctors have always been baffled by patients’ different response to the same treatment.
Thankfully, advancements in technology and genetic testing have now made the following three key things clear about cancer:
- Genetic changes in cells are responsible for the extent of growth and spread of cancer.
- The same cancer-causing changes may be present across different cancers.
- Genetic changes that affect one individual with cancer may not necessarily affect others with similar cancer.
With the given knowledge about cancer and its associated mechanism, there is not a consensus among scientists that a more personalized and individualized approach is needed for the treatment of cancer patients. This article talks about precision medicine and its applications in cancer treatment.
Part 1: Precision Medicine in Cancer Treatment: Current Scenario
Currently, a cancer patient is required to undergo extensive testing to identify the extent, stage, and grade of cancer. Based on the reports, a team of oncologists decides the course of treatment. Every patient is likely to receive a combination of treatment, which may include chemotherapy, surgery, radiation therapy, immunotherapy, or hormonal therapy.
Even though it is now known that specific genetic changes in the cells cause cancer. However, genetic testing to identify the type of changes in the DNA of the cells is not conducted for every patient. In fact, they are made to undergo several cycles of chemotherapy and radiation therapy, following surgery for the removal of the tumor and the nearby tissues.

Source:https://www.cancer.gov/
This is partly because there is no way for the doctors to realize whether a particular treatment would work for a patient or not. Therefore, they follow a standardized and most common approach for cancer treatment.
However, things won’t be the same in the near future. There is a hope that in the future, cancer treatment will be more individualized and based on the actual genetic changes in each person’s cancer. Thanks to advancements being made in the field of molecular biology, there will be extensive genetic testing in the future that will help scientists prepared drugs that directly target those changes.
Accordingly, the doctors will be able to prepare a treatment plan that is most likely to suit the patient with the given genetic changes, This way, there will be no need to undergo repeated cycles of chemotherapy, radiation therapy, and other treatment modalities that are least likely to benefit the patient.
Currently, researchers around the world are carrying out studies to test whether treatments that target the genetic changes directly will help cancer patients, irrespective of the site of the tumor. While precision medicine is expected to become a mainstream medicine in the near future, a part of it is already in practice.
There are several drugs that have already been approved by the Food and Drug Administration in the US. These drugs directly target genetic changes in the cells, based on the type, size, and the region of the spread of cancer. The use of drugs to target the changes in the DNA is also known as targeted drug therapy
Precision Medicine in Breast Cancer Treatment
Precision medicine has been in use for many years in breast cancer treatment. For example, treatment for breast cancer patients is personalized on the basis of whether they have HER2-positive breast cancer or estrogen-and progesterone-positive breast cancer.
Several clinical trials have been conducted in the past to figure out therapies that work the best for specific groups of people. If you belong to a particular group, you are most likely to be given treatment or therapies that work the best for that particular group.
For example, patients with HER2-positive breast cancer are most likely to receive targeted therapy using the drug trastuzumab, which is also known as Herceptin. This drug is known to lower the risk of cancer recurrence after the initial treatment. Therefore, if you have HER2-positive breast cancer, your treatment plan is expected to be personalized to include Herceptin.
Source: Wikimedia commons/RedAndr
Similarly, breast cancer cells are also tested for hormone receptor status. Breast cells possess hormone receptors for estrogen (ES) and progesterone (PR). These receptors may or may not be present in breast cancer cells. If the receptors are present, the patient is likely to receive hormone therapy.
Hormone therapy includes the use of specific hormones that work by blocking the receptors from attaching themselves to the respective hormones. Thus, the treatment plan for ER-positive and PR-positive patients is personalized. On the other hand, ER-negative and PR-negative patients are not likely to benefit from hormonal therapy.
Several targeted therapy drugs are under trial for the treatment of breast cancer. These therapies are being studied for the treatment of metastatic breast cancer, and the findings of these studies will help determine whether the drugs are suitable for the treatment of early breast cancer patients.
A few drugs have already been approved and are currently a part of standard treatment for specific risk groups. Targeted therapy drugs work by targeting certain cellular pathways or cancer cells directly. Specific classes of targeted drugs, including poly (ADP-ribose) polymerase (PARP) inhibitors and tyrosine-kinase inhibitors are currently being used for the treatment of metastatic breast cancer.
Major Goals of Precision Medicine in Cancer Treatment
Some of the main goals of precision medicine in cancer treatment are to:
- Figure out the most effective treatment for the cancer patient.
- Avoid unnecessary treatment that is less likely to work in the case of specific groups of patients.
- Avoid unnecessary side effects, trauma, and risks of breast cancer surgery.
- Identify people who are most likely to respond to a particular cancer therapy.
- Develop therapies that target specific tumor cells or cellular pathways.
Precision medicine especially focuses on cancer treatment. This is because the development of precise and effective treatment strategies for cancer patients can help improve their quality of life. Additionally, it will help bust the long-standing “one-size-fits-all” myth for cancer treatment.

Source: Alton Calsoft Lab
Precision medicine should be, in fact, a major focus when it comes to cancer treatment. This is because each cancer patient has a different genetic profile and this profile can change from time to time. Therefore, they will be more benefited when a treatment plan is prepared as per their individual needs.
So, what does personalization for cancer patients actually mean?
Personalization of cancer treatment has a different meaning for each patient. Personalization may come in different forms, and this may include:
- Cancer testing to determine whether a particular cancer treatment will be effective for a patient or not.
- Genetic profiling to understand whether the patient can handle a particular medicine or hormone.
- Assessment of genetic composition of the mutation to identify the degree of cancer risk.
Does precision medicine apply to everyone?
Even though several drugs have been made that target specific mutations, there is no drug that targets all patients of a specific cancer type. Therefore, if there is a targeted drug therapy available for cancer that you are suffering from, you will still be required to undergo genetic testing to figure out whether you have the possess the changes that are targeted by that particular drug. Therefore, the answer is clear. Precision medicine does not apply to everyone.
Part 2: Technologies That Support Precision Medicine
Precision oncology has made significant changes in the way how patients are treated now, but it still has a long way to go. This long journey will be made easier by the influence of new technologies that allow researchers to identify specific targets for precision oncology.
The following are the two promising technologies that will undoubtedly support precision medicine and its applications in cancer treatment:
CRISPR/Cas Technology
CRISPR/Cas technology is also known as the gene editing technology. It allows the insertion, deletion, and exchange of DNA sequences. The difference between spontaneous mutation and the use of this technology is that the exchange of genetic material in the latter case takes place in a controlled environment. This is why this technique can be used to create animal models that mimic the genetic changes in the cancer patients. By studying the animal models with the same genetic mutation, the scientists can actually figure out which drugs or treatment modality is most likely to benefit the patient.
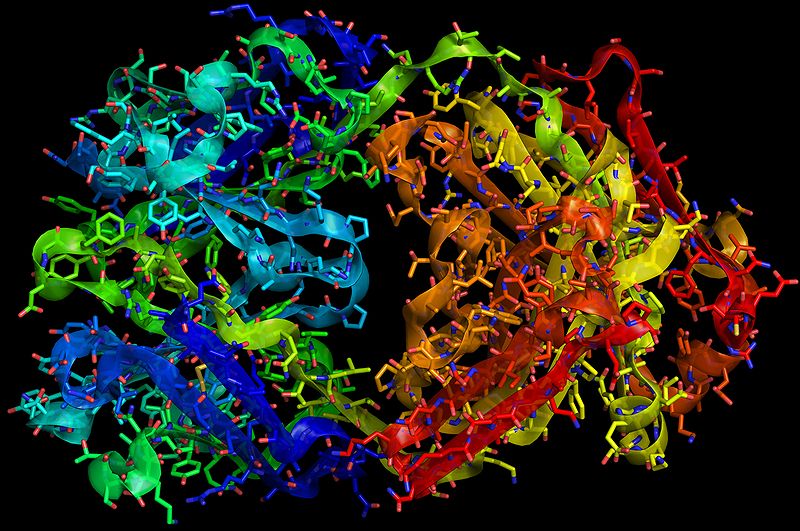
Cryo-electron Microscopy (Cryo-EM)
Cryo-EM is a special type of transmission EM in which the samples are examined at extremely low temperatures, that is, at cryogenic temperatures. At this temperature, the proteins and the viruses are frozen, and therefore, it is easier for the researchers to accurately study the biological events at an atomic level. It also helps researchers understand the possible results of genetic changes in drug resistance and response.
Source: Wikimedia Commons/J LEVIN W
Tech Giants Supporting Personalized Treatment
There are several tech giants such as Microsoft, Google, and IBM that actively participate in cancer research. These companies, along with several other start-ups are designing novel artificial intelligence solutions that can be used to provide personalized treatment to cancer patients.
Microsoft’s machine-learning project called “Hanover” intends to predict the combination of drugs that will work the best in case of patients with a specific tumor type, grade, and stage. On the other hand, there is a Swiss company called Oncompass that biopsy analysis of samples derived from an oncology patient so that the doctors can prepare a personalized treatment plan for the patient.
There are several other countries that offer attractive packages to patients who have been advised whole genome sequencing, genetic testing, and interpretation. The Boston-based company, Veritas Genetics, is one such company that also offers a myBRCA HiRisk test, which is a genetic test that calculates a women predisposition to ovarian, breast, and other related cancers.
Part 3: Effectiveness of Precision Medicine
There are many critics of medical innovations around the world that have constantly argued that such technologies are over-hyped and medical professionals must stay careful with the extent and use of such tools. The same is true about precision medicine as well.
Precision medicine has been downgraded a number of times in the past. While it is true that digital health experts may get overly excited about a new technology and that the bad effects of over-hyping, the prospects of precision medicine are vast and should not be underestimated.
What once seemed a distant possibility in the medical world is now a reality, thanks to the newer innovations in the first of technology. There are software and algorithms that can actually be used to map mutations and associated them with treatments that are most likely to work faster for patients. The cost of genome sequencing has reduced from millions to thousands, and now it is possible to derive cancer cells from the blood of the patient for analysis than to take a tissue sample for biopsy.
Technology is, therefore, expected to bring a lot of positive changes in how treatment is delivered to cancer patients. The same is the case of precision medicine, which is all set to become a part of the mainstream medical practice in the coming years.
Potential Benefits of Precision Medicine
- The wider ability of the doctors to use patient’s genetic and other molecular information as a part of routine medical care.
- Chance of incorporate patient’s personal preferences to specialize a treatment plan.
- Extended survival rate, especially in the case of cancer patients.
- Improved ability to predict which treatment will work best in a specific patient.
- Design of new tools for building and analyzing treatment data.
- A better understanding of the underlying mechanism causing the disease.
- Reduction in the total cost of treatment.
- Fewer side effects and avoidance of unnecessary treatment.
Part 4: Use of Precision Medicine
The US has been moving quickly towards the world of precision medicine. There are several consumer-facing organizations that already offer the patients a chance to have a look at their genetic data. On the other hand, there are institutions such as Geisinger’s Genomic Medicine Institute that is pro-actively collecting the genetic data of their patients. Such forward-looking companies, facilities, and health systems are propelling precision medicine in the right direction.
There has been a significant shift in the way how laboratory systems around the world have been incorporating precision medicine. This has been especially true about the US laboratories. There has been an increase in the number of hospitals that have deployed advanced laboratory capabilities such as precision medicine (molecular diagnosis), laboratory – outreach services, transfusion management system, and specimen collection management system.

Source: HIMSS Analytics
According to HIMSS Analytics, nearly 80 percent of the oncology hospitals in the US deployed precision medicine by 2012. In the year 2016, nearly 50 percent of the academic hospitals in the country had deployed precision medicine.

Source: HIMSS Analytics
Thus, oncology continues to remain one of the largest areas of focus for providers who are willing to invest in personalized medicine. Cardiology stands second with 50 percent respondents reporting the use of genomics for diagnosis and treatment of heart conditions, followed by nephrology and endocrinology.

Source: HIMSS Analytics
As per HIMSS Analytics, more than 62 percent of the survey respondents confessed that precision medicine diagnostics and treatment is already in use at their respective organizations.
The University College of London (UCL) Institute for Precision Medicine has been quite instrumental in accelerating the development of new therapies and drugs for personalized medicine. Developmental neurosciences, neurotransmitter gene therapy, stem cell therapy, ophthalmology gene and cell therapy, molecular and cellular immunology, and gene therapy for metabolic diseases are some of the areas of research that the institute is currently exploring.
The institute is equally instrumental in the development of new biochemical and genetics diagnosis for both common and rare diseases. There is a dedicated team that takes care of advances in genetic profiling, which includes sequencing, validation, epigenetics, and pharmacogenomics and how this branch of science can be used to diagnose, treat, and prevents diseases as per individual’s unique genetic profile.
Part 5: Efficacy of Precision Medicine
Several research studies are being continuously conducted to see the effectiveness of precision medicine in different specialties. One such study conducted by a team of researchers from the University of California San Diego indicated that using treatment approach that entails precision medicine can actually prolong remission rates while improving patient health.
The study, originally published in the journal JAMA Oncology, was conducted on the two groups of patients. For the first group of patients, biomarker-based selection strategy was used to administer cancer treatment. The second group of patients received routine or traditional treatment.
The researchers observed significantly improved outcomes in Group 1. The response rates were as high as 30 percent in patients treated with precision medicine. However, the second group did not respond favorably to the traditional treatment. The response rates were only 4.9 percent in such patients.
Additionally, the disease remission rates in the first group were much higher than the second group. Patients treated with precision medicine remain disease free for almost 5.7 months, while those treated with traditional medicine saw just 2.95 months of progression-free survival on an average.
Part 6: Precision Medicine in Action (Apart From Oncology)
Doctors have always been aware while prescribing medicines to patients that there is no medicine that affects every patient in the same manner. Yet, trial and error have almost always been the method of knowing which medication will work in the case of a patient.
But this has changed quite a bit in the recent past, thanks to advances in the branch of precision medicine called pharmacogenomics. This branch aims to identify how individuals with specific genetic variations are likely to respond to the given medications.
Regenerative medicine is one example of precision medicine in action. Stem cells manipulation is one thing, but the entire branch becomes even more powerful when it is combined with advanced technologies such as 3D bioprinting and engineering. There are several stories of patients that have already received replacement bladders and engineered blood vessels and bones. This is only possible through precision medicine, which is personalized as per the individual needs.
Another example of precision medicine at play is the generation of computer algorithm-based personalized diet plans. Such diets generated by the computer based on specific data and personal details are found to be as effective as the diet plans shared by an expert dietician.
There are many such examples of precision medicine in action today. The different approaches to precision medicine are likely to be made available to people in the next couple of years.