Referrals and Prior Authorizations are a headache for most referral coordinators in health systems throughout the United States. Below are a few statistics documenting the financial risks to your healthcare organization, your patients, and providers which stem from poorly managed physician referrals.
Photo by valelopardo on Pixabay
1/3 of Patients and $1.7M
- A third of patients are referred to specialists each year. Each referring provider represents $1.7 million in potential revenue for destination providers. What is getting in the way of a strong referral network?
Referral Workflows are Inefficient and Unreliable
- Nearly 20M referrals are considered clinically inappropriate each year. Increasing risk of payment denial or delay.
- 46% of faxed referrals never result in a scheduled patient visit.
- 52% of specialty referrals are unnecessary
Systems Fail to Coordinate Outpatient Care
- Up to 50% of physicians’ referrals are not tracked.
- $1.9 billion is incurred annually by patients in lost wages and co-pays, increasing patient frustration.
Inefficiency Leads to Scheduling and Payment Delays
- 63% of physicians wait several days to receive insurance authorizations.
- $31 Billion is spent each year interacting with health insurance companies regarding payments and authorizations.
So how do you become the preferred provider?
- Connect your entire physician community with an end-to-end referral management workflow software application from ReferralMD.
- Give providers fast and reliable care coordination experience that is convenient for staff and patients alike.
- Integrate revenue cycle steps upfront to avoid payment delays, secure authorizations, and facilitate timely payment.
Provider Survey Data

ReferralMD pulled research from the Reaction ecosystem on 549 independent physicians to understand how they choose a destination provider for their patient referrals. Most surveyed say they don’t currently have a preferred hospital partner, giving health systems a great opportunity to become the preferred partner for independent physicians.
According to recent data from Accenture, seven percent of patients have switched healthcare providers due to a poor customer experience, which results in a loss of more than $100 million in annual revenue per hospital. Additionally, U.S. hospitals spend more than $1.5 billion annually on advertising. Yet, much of this is lost if providers and patients who want to do business with the hospital cannot easily do so. Below are insights to help make a hospital a referral destination of choice.
Key Takeaways
- Opportunity Knocks: More than half of physicians don’t have a preferred hospital partner, which means many hospitals do not realize the full economic value of community partners.
- Time-Saving Services Attract: It’s easier than you think to attract independent providers with convenient services – nearly 40 percent want insurance authorizations and self-scheduling.
- Convenience is King: Roughly half of the independent physicians put a high value on patient preference and convenience in their choice of hospital.
Learn more about ReferralMD’s centralized referral management solution.
Independent Physician Survey Results
Physician Preferences for Hospital Partners
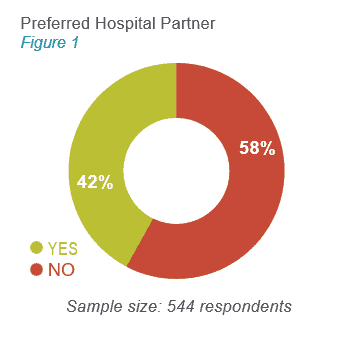
Does your organization have one or more preferred hospital partners?
Forty-two percent of surveyed physicians said yes, but a majority (58 percent) said no (see figure 1). This means hospitals have not gained the full economic value of their community partners, resulting in an opportunity to become the referral destination of choice. Hospitals face dual pressure from competition and the move to value-based payment. It’s more important than ever to provide outstanding value to referring providers’ patients and be easy to do business with from both the provider and patient point of view.
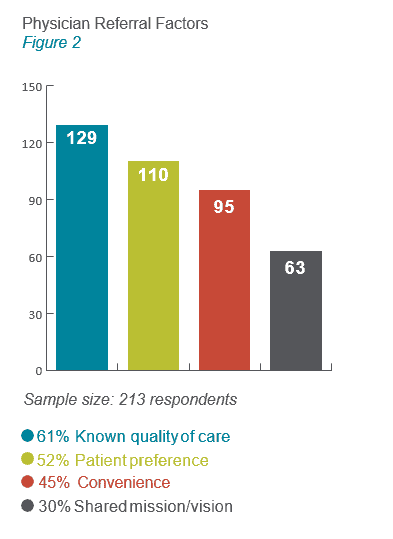 What are the most important factors for determining where to refer patients?
What are the most important factors for determining where to refer patients?
Physicians value shared mission and commitment to quality care for their patients. In today’s changing market, convenience – for patients, as well as referring providers – will drive patient preference and continue to increase in importance (see figure 2). Patient expectations continue to evolve as they use services like Uber, Airbnb, and Amazon, influencing their expectations for how their healthcare interactions should work. Hospitals and their physician partners who provide convenient, patient-focused care coordination and access will be competitive.
Hospital Partners Gain Volume
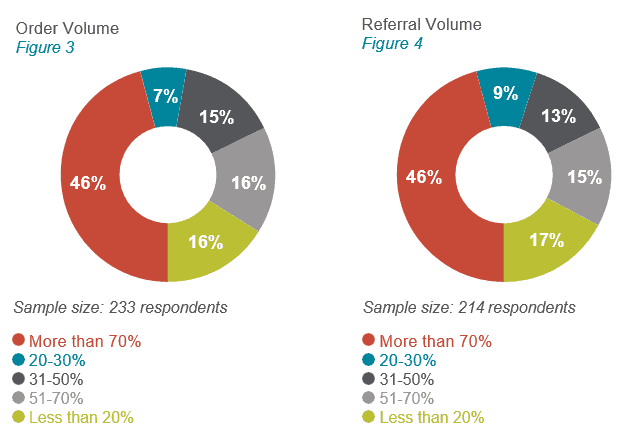
What percentage of order and referral volume is going to top hospital partners?
Of those who have preferred hospital partners, 46 percent of physicians said that more than 70 percent of their orders go to top partner(s) (see figure 3). Forty-six percent also said more than 70 percent of their referrals go to top hospital partner(s) (see figure 4). These results reinforce that referring physicians will continue to send patients to that hospital once a convenience and service is established with a preferred destination hospital.
Value of Physician Services
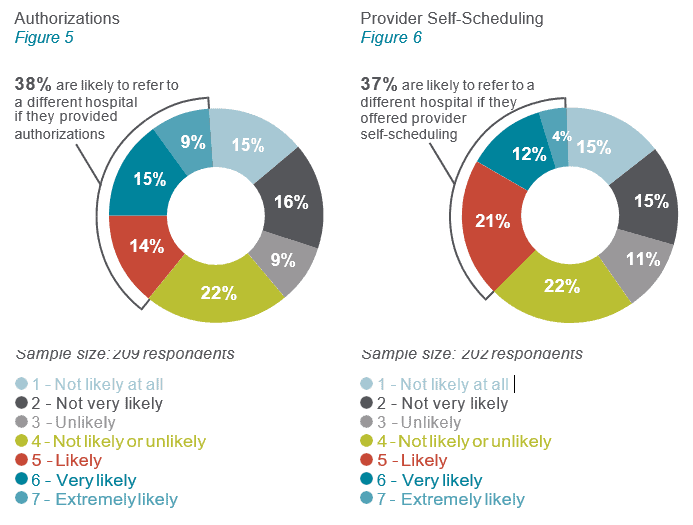
How important are authorizations and self-scheduling options?
Thirty-eight percent of physicians are likely to refer to a different hospital if the hospital provides Authorizations (see Figure 5). Thirty-seven percent are likely to refer to a different hospital if the hospital offers community providers self-scheduling tools (see figure 6).
If you adopt these two functions well, you will be more attractive to referring providers. More than ever, providers and their patients expect smooth care coordination regarding referrals, orders, authorizations, scheduling, and payment.
What are the most important self-scheduling features?
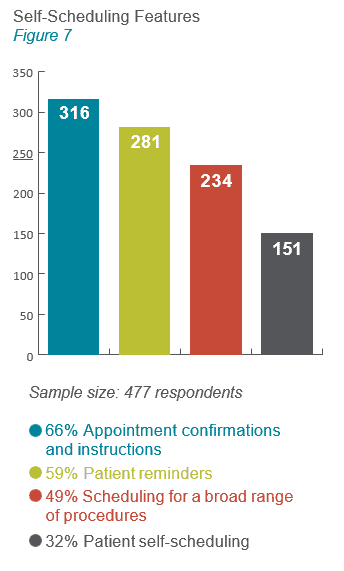 Convenience and good communication are themes in these self-scheduling features (see figure 7). Physicians want to refer patients to hospitals that are easy to work with, provide communication back to them about their patients, and make the experience smooth and convenient. Similarly, today’s healthcare consumer expects easy access and engagement when dealing with the healthcare system. A recent Accenture report found that 77 percent of patients think the ability to book, change or cancel appointments online is important. Yet, only 2.4 percent of appointments today are patient self-scheduled.
Convenience and good communication are themes in these self-scheduling features (see figure 7). Physicians want to refer patients to hospitals that are easy to work with, provide communication back to them about their patients, and make the experience smooth and convenient. Similarly, today’s healthcare consumer expects easy access and engagement when dealing with the healthcare system. A recent Accenture report found that 77 percent of patients think the ability to book, change or cancel appointments online is important. Yet, only 2.4 percent of appointments today are patient self-scheduled.
ReferralMD used data collected through Reaction’s platform, a Research as a Service ecosystem with access to more than 500,000 healthcare.
To author this report. The results include survey responses from 549 independent physicians in the U.S. – www.reactiondata.com