Healthcare Technology is changing fast, but maybe not as quickly as we would hope. Is 2021 the year health systems and insurance companies decide that they can no longer wait for the slow solutions and they jump on the software technology bandwagon? (IT departments I am pointing at you). It’s time healthcare providers started getting creative with technology and help their staff spend less time doing manual labor (cough the fax machine). The world is changing, are you ready to read the top Healthcare Technology Innovations?
Also: We’ve updated our FREE medical marketing strategy ebook. Click here to Download.
Healthcare Technology Acquisitions on the Rise
This is going to be an exciting year for healthcare technology as mergers and acquisitions are heating up. Back in 2017 alone, there were 43 acquisitions with Internet Brands acquiring WebMD leading the way at $2.8B.
So what does this mean for the future of insurance companies, health systems, startups, and patients?
It means we finally may see some significant changes in how healthcare is administered, improvements in patient access, lower wait times, improved revenues for health systems, lower costs, and much more.
But hopefully, the healthcare industry will not remain frozen in time for much longer.
Learn more about ReferralMD’s Referral Management Solution
What are the top healthcare technology innovations?
We have personally researched the web for a year to find the best companies that are making a difference and have compiled an amazing list below. Here’s to change!
1. Payer-Provider Analytics/Data software
Blurring Lines between Insurance Companies and Physician Practices
Several carriers are already are giving healthcare organizations claims data, analytics, and tools to help make better decisions on which providers are “more appropriate” based on quantitative data, not “Yelp reviews.”
It all boils down to high-quality data, and who has it.
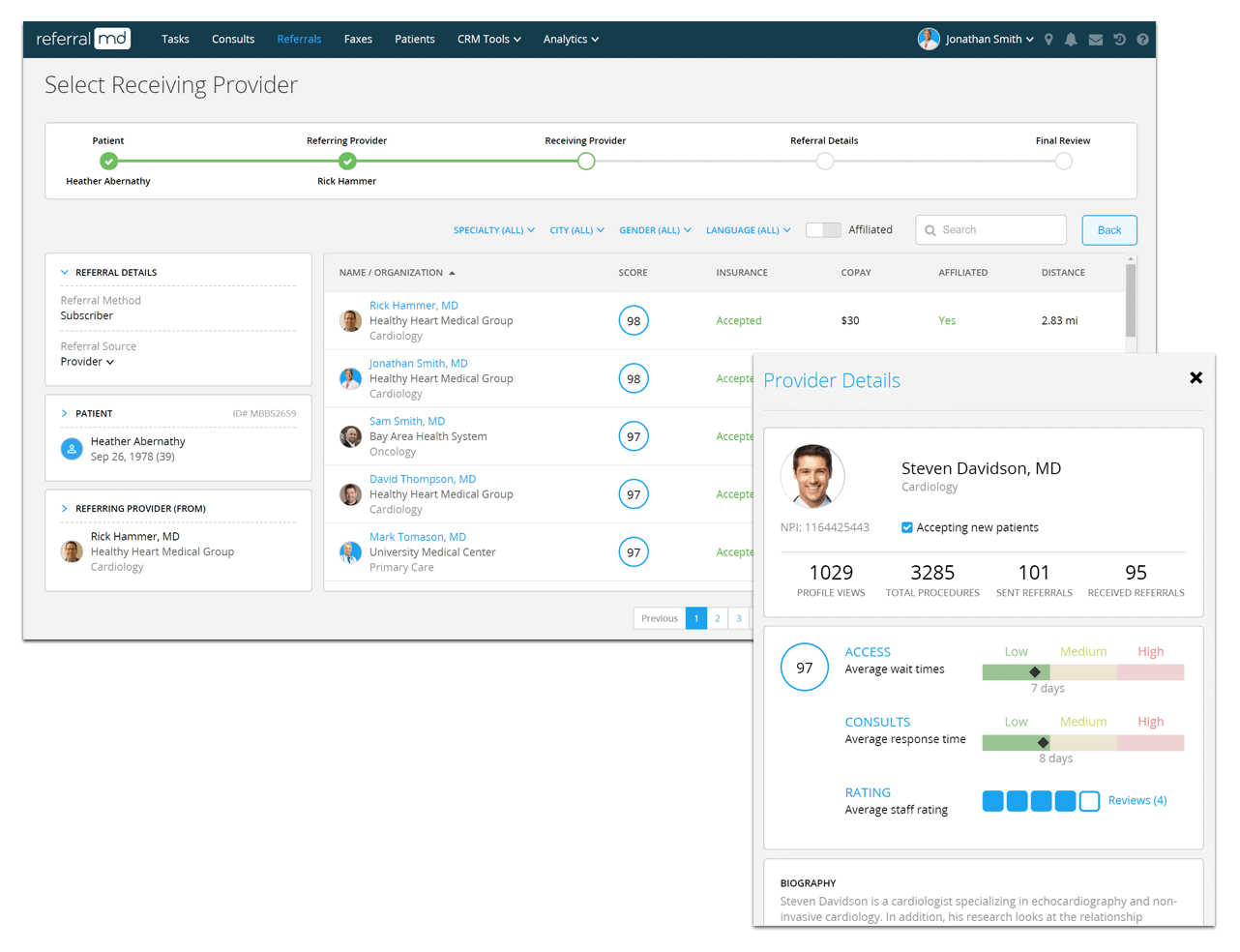
An example of how this is used in a care coordinator’s workflow is when a patient is about to be transferred to a specialist after an initial screening at a PCP or insurance company. The coordinator at the point of care has full visibility to their referral network, provider affiliations (in-network status), accepted insurances, proximity to the patient, experience of the doctor, and even ranks the specialist on a quantitative score from 1 to 100.
The True Cost of Patient Leakage
- More than 200,000 physicians in the U.S. are now employees, and 3 in 4 medical residents will start their careers as employees of a medical group, hospital or faculty. As healthcare organizations continue to consolidate and build larger networks, better collaboration between primary care and specialists is critical.
- With only 35% to 45% of referrals for adult inpatient care, as measured by revenue, go to a partner hospital. This results in over $90M dollars in revenue loss for every 100 employed physicians due to care teams not having accurate information about their specialty care network.
When patients receive out-of-network care:
- The ability to coordinate care is dramatically decreased, which in turn can undermine patient outcomes and population health management efforts.
- The network loses both clinical and financial control of the patient’s care. For example, an out-of-network physician may order tests and treatments that do not align with evidence-based best practices. Regardless, the parent network is still responsible for the cost. In this case, patient leakage can significantly increase the cost of care.
Healthcare Technology tools like ReferralMD’s referral management and patient consult software can optimize decision support, improve workflow, and reduce leakage.
Competitor Analysis
Referral data can also be used by physician liaisons to look up which competitors receive the most referrals in certain geography based on specialty, city/state, procedures offered and more to learn which organizations could make the best partners based on referral volume. Another option is to look up your own doctors to see if they are steering patients to competitors.
How much are you losing to out-of-network referrals (Leakage)?
Apply to Receive your Free Competitor Analysis Report
2. Artificial Intelligence
While promising, AI is still in its infancy but holds promise as healthcare technology for patients today that wish to schedule doctor appointments based on the severity of the symptoms, minimize staffing challenges, monitor the health status, and notify a human nurse immediately if the parameters are out of control, helping homecare assistants stay informed about patients’ evolution.
Here are a few applications that come to mind out that I feel are doing an amazing job with Artificial Intelligence.

- Cerebro – AI for Nurse Staffing – Day and night, hospitals require high-quality clinical staff for their patients. To meet their needs, hospitals increasingly rely on inefficient, insufficient staffing agencies. The agencies rarely find all of the necessary staff or only after a long delay. At the same time, agencies treat themselves to high margins instead of rewarding the clinicians’ valuable work.
Cerebro offers a solution: a faster, responsive healthcare labor marketplace — one that connects healthcare facilities with verified, ready-to-work clinicians. Specifically, Cerebro offers acute care facilities:
- Faster fill times. Clinicians on the Cerebro platform use a mobile app that enables them to find and request shifts. It’s fast and easy. The app also uses AI to notify clinicians of new assignments that are an especially good fit.
- Higher fill rates. Clinicians on Cerebro can expect to pay up to 30% more than with staffing agencies because Cerebro takes a smaller commission than traditional agencies. Hence Cerebro can attract a larger pool of talented clinicians.
- Staffing flexibility. Fill for 1 shift, 1 week, or 1 month. Cerebro does not require minimum contract times. Hospitals find the staff they need when they need it; clinicians work the hours they want when they want it.
Most of us are used to chatting with our phones using Siri about the latest sports scores, or Alexa to turn on music, but how comfortable are we discussing private medical issues with chat-bots that may store the information in their database. Here are a few more companies that come to mind…
- The company, Kore.ai offers smart bots for healthcare facilities. The digital assistant can connect patients to the right contacts directly, give appointment details or make any changes. It lets the patients easily refill prescriptions or pay bills. It delivers lab, test or procedure outcomes or recommended next steps.
- Safedrugbot embodies a chat messaging service that offers assistant-like support to health professionals, doctors who need appropriate information about the use of drugs during breastfeeding.
- Izzy helps women track their period and serves as a birth control pill reminder.
3. Blockchain as an emerging Healthcare Technology
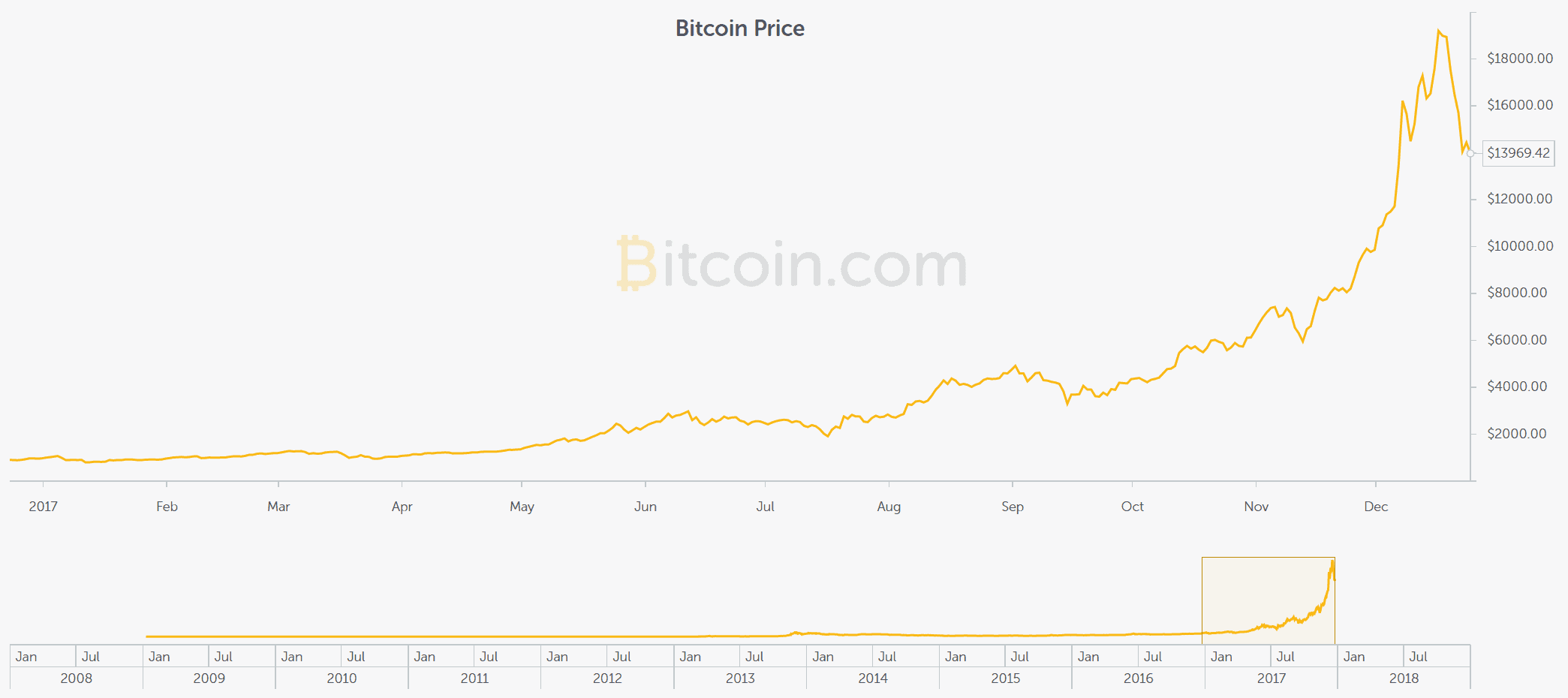
You have probably heard about Bitcoin and its explosive growth from $.08 cents in 2009 to almost $20,000 dollars in 2017. It uses blockchain technology to exchange information with others.
So what is blockchain you may ask?
Effectively a blockchain is a kind of independent, transparent, and permanent database coexisting in multiple locations and shared by a community. This is why it’s sometimes referred to as a mutual distributed ledger (MDL) versus a single client-server database like your standard website where one owner controls the access credentials.
So how does blockchain apply to healthcare?
The end goal would be a decentralized record system using blockchain independent of EMR’s controlling the data. But as we know this will not happen until a government mandate or EMRs opening up their data silos.
How bad is communication in healthcare?
There are 26 different electronic medical records systems used in the city of Boston, each with its own language for representing and sharing data. Critical information is often scattered across multiple facilities, and sometimes it isn’t accessible by either the patient or doctors, when it is needed most—a situation that plays out every day around the U.S., costing money and sometimes even lives. But it’s also a problem that looks tailor-made for a blockchain to solve, says John Halamka, chief information officer at Beth Israel Deaconess Medical Center in Boston.
While it would be massively beneficial to patients and providers alike, it looks like the fax machine is here to stay for another 10 years.
4. Internet of Medical Things (IoMT)
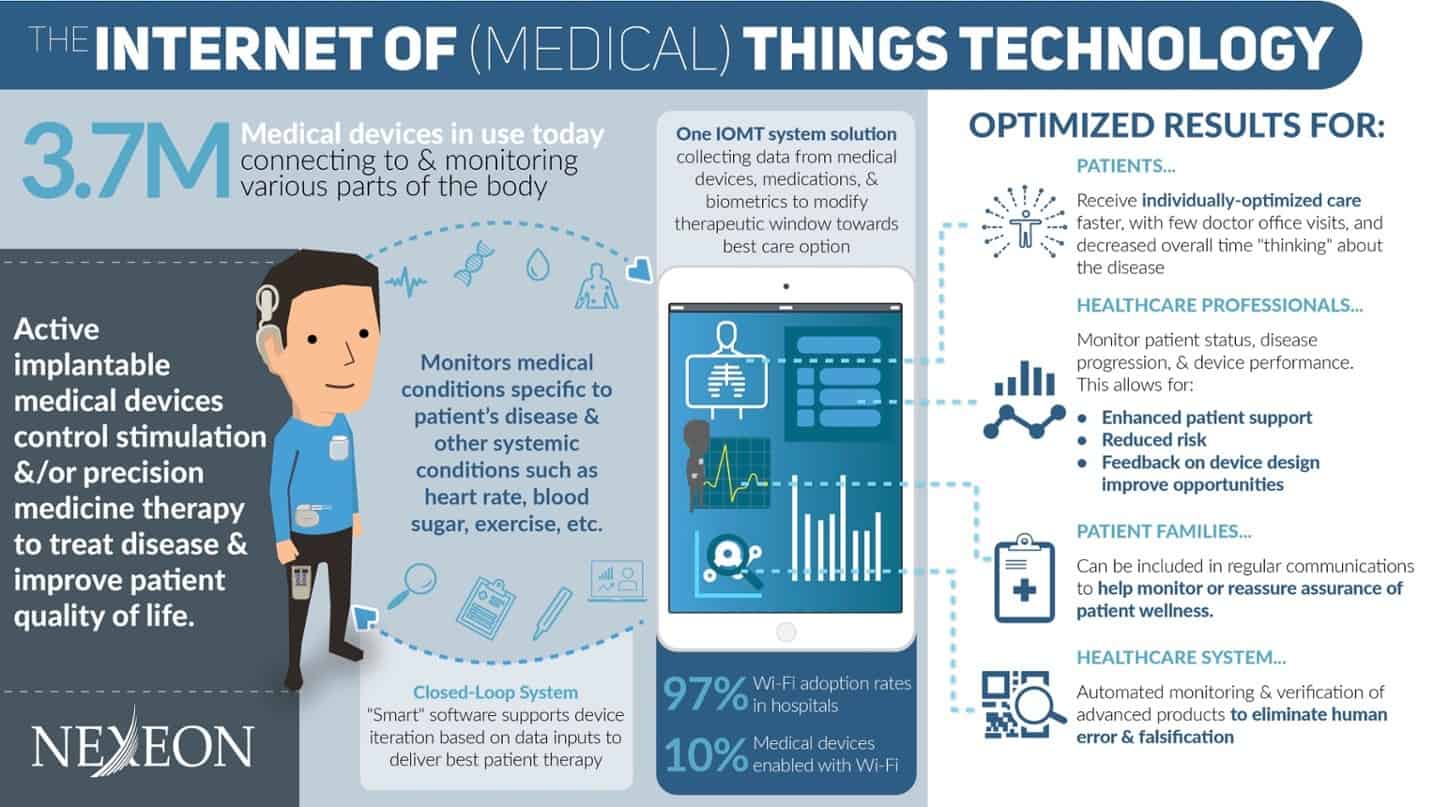
Internet of Medical Things, or Healthcare IoT, refers to a connected infrastructure of medical devices and software applications that can communicate with various healthcare IT systems.
As an example, this can be thought of as simple as someone who wears a FitBit to track his or her steps; that step count is tabulated on an iPhone via Bluetooth technology, and then that data can be shared with a physician to provide feedback via Wi-Fi connection and automated reporting data, and it can also send that data to your closest friends and family.
What are the dangers of IoMT?
The greatest danger related IoMT is the high barrier to entry to truly disrupt the healthcare industry and to change the way disease is treated. There is a threshold for the speed at which anyone can execute on delivering these innovative solutions to a population and industry that so desperately need change.
Regulatory hurdles
With each change inherent in the introduction of these systems, there are massive regulatory hurdles that require significant amounts of resources, even more so than a typical medical device pathway to commercialization.
And beyond the historically proven 10 years and $30M to take a MedTech product to the US market, there is the added burden of competing in a commercial space against pharma and other MedTech conglomerates that have 1000x more resources and power to squash any new competition, even if the solution is what’s best for the patient.
One of the latest announcements from The Centers for Medicare & Medicaid Services (CMS) confirms that the largest payer in the U.S. sees remote patient monitoring (RPM) as part of the future of care delivery. Why? Because next year, they will begin incentivizing the use of connected technology to capture patient-generated health data.
Since January 1, 2018, clinicians have used the newly unbundled reimbursement code CPT 99091 to bill for the time they spend reviewing and interpreting data collected or transferred by a remote monitoring tool. The changes to this code will have significant implications for accelerating the adoption of remote monitoring tools into clinical practice.
How can clinicians position themselves to take full advantage of this new incentive, understand the changed guidelines, and determine how RPM could be incorporated into their practices?
What are the benefits of IoMT?
The benefits of introducing IoMT are vast, and certainly, there are even more benefits to be discovered as we continue to grow our expertise in this space as an industry. But to name a few:
Objective reporting: Because the devices can record and report on actual activity at the level of the nervous system, we no longer have to rely solely on subjective patient reports of “how they are feeling”; instead, we have an objective evaluation of the disease progression and patient therapy efficacy as reported by the devices,
Remote monitoring: Increased patient accountability as the healthcare provider will have a “report card” so to speak of actual patient therapy compliance instead of relying on the accuracy of patient summary,
Local activity recording: Device recording capabilities allow for the collection data that we’ve never previously been able to access. This data will vastly improve our understanding of the mechanism of action of these chronic diseases. And if we understand the disease better, we will undoubtedly enhance our approach to disease prevention and therapy,
Automation: The automation of device and therapy records decreases human error or fraudulent reporting within hospitals and sub-acute care facilities,
Precision medicine: the delivery of targeted stimulation that is optimized for that individual facilitates improved therapy with decreased undesired side effects. When you take a pill, for the most part, that pill is metabolized in some fashion and then distributed systemically throughout your body regardless of its intended target. While there are many advances to decrease these drug-related side effects, the level of precision we can achieve with devices that can steer stimulation to a specific target is of a much higher degree,
Adaptability: Because our systems are built on a feedback loop, the system iterates on that feedback and adjusts for improved patient outcomes.
Which Companies are Leading the Way?
One company that we feel is changing the game is Noteworth, a connected health platform that enables health organizations to prescribe virtual care models to their patients. They help clinicians collect and access contextualized patient-generated health data that improve care coordination and outcomes, reduces costs, and better engages patients.

Noteworth Dashboard
- Easily prescribe tailored virtual care models to your patients and assign accompanying care instructions to them.
- Receive visualized, usable patient-generated health data in continuous Noteworth Reports you can monitor at any time.
- Set customizable alerts, called Focus Notes.
- Streamline your documentation and optimize towards reimbursement goals with the Encounters tracker.
5. Update from 2017 – Tricorder XPrize
As you may have read from our previous ReferralMD Healthcare Article, Final Frontier Medical Devices was awarded $2.5M from Qualcomm to continue improving their device and bring it to market.
More about the company:
Final Frontier Medical Devices, a Pennsylvania-based team led by brothers Dr. Basil Harris, an emergency medicine physician, and George Harris, a network engineer, took home the 1st place for their artificial intelligence-based engine, DxtER, that learns to diagnose medical conditions by integrating learnings from clinical emergency medicine with data analysis from actual patients. DxtER includes a group of non-invasive sensors that are designed to collect data about vital signs, body chemistry, and biological functions. This information is then synthesized in the device’s diagnostic engine to make a quick and accurate assessment.

6. Breast Cancer Drug – Abemaciclib
One in eight women will be diagnosed with breast cancer in her lifetime. First-line cancer DNA-creating proteins often get dismantled by chemotherapy, but BRCA genes have a backup plan that repairs the DNA and is carried out by poly-ADP-ribose polymerases (PARPs).
Eli Lilly’s breast cancer drug Abemaciclib is all set to hit the market very soon. It belongs to CDK4/6 inhibitors which have been shown to have the most positive effect on metastatic breast cancer, specifically in HER2+ breast cancers. Abemaciclib is armed with certain advantages over its rivals — Pfizer’s Ibrance and Novartis’ Kisqali — as it can be dosed continuously. The clinical studies results have put Abemaciclib roughly on par with its competitors in the first-line setting.
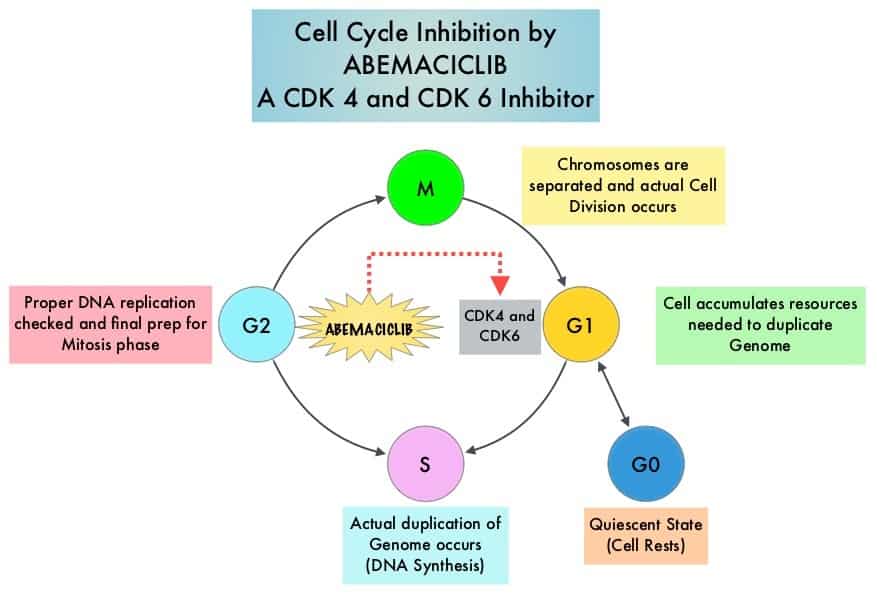
Updated results from MONARCH3 studies have bolstered the potential for this drug to be in the best-in-class category of cancer drugs. In July 2017, the U.S. Food and Drug Administration (FDA) granted Abemaciclib a Priority Review tag, both as a potential monotherapy and combination therapy. Abemaciclib entered the market in 2018 and captured a significant market share in this space. Sales are estimated to approach USD 1,792 million in 2022.
7. Patient Engagement (see also: how to change your EHR)
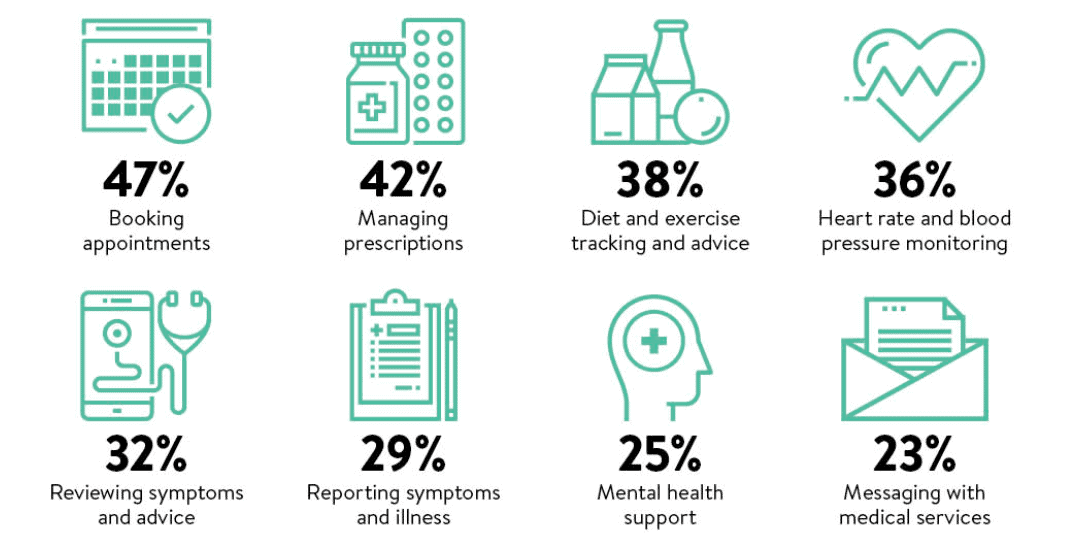
- The global patient engagement solutions market is expected to grow at a compound annual growth rate of 16.2% over the next five years, reaching $18.7 billion in 2022, according to MarketsandMarkets.
- Driving the growth is an aging population, the increasing burden of chronic diseases, and a push to get patients to assume more responsibility for managing their care.
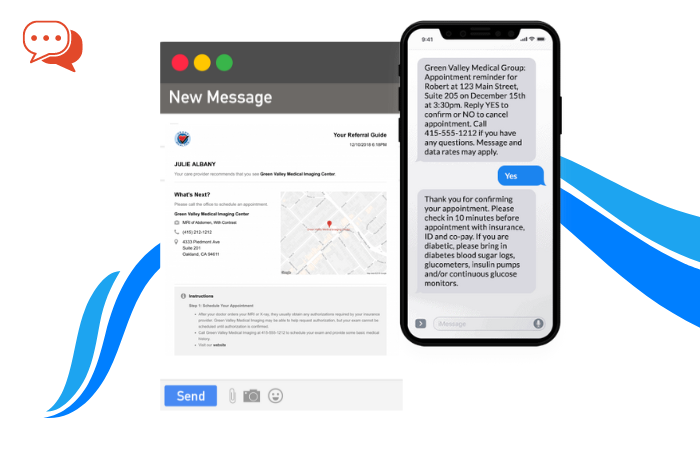
- While patient engagement tools can enhance communication and help to improve outcomes while reducing costs, barriers such as patient data security and lack of interoperability persist and could prevent the market from reaching its full potential, the report says.
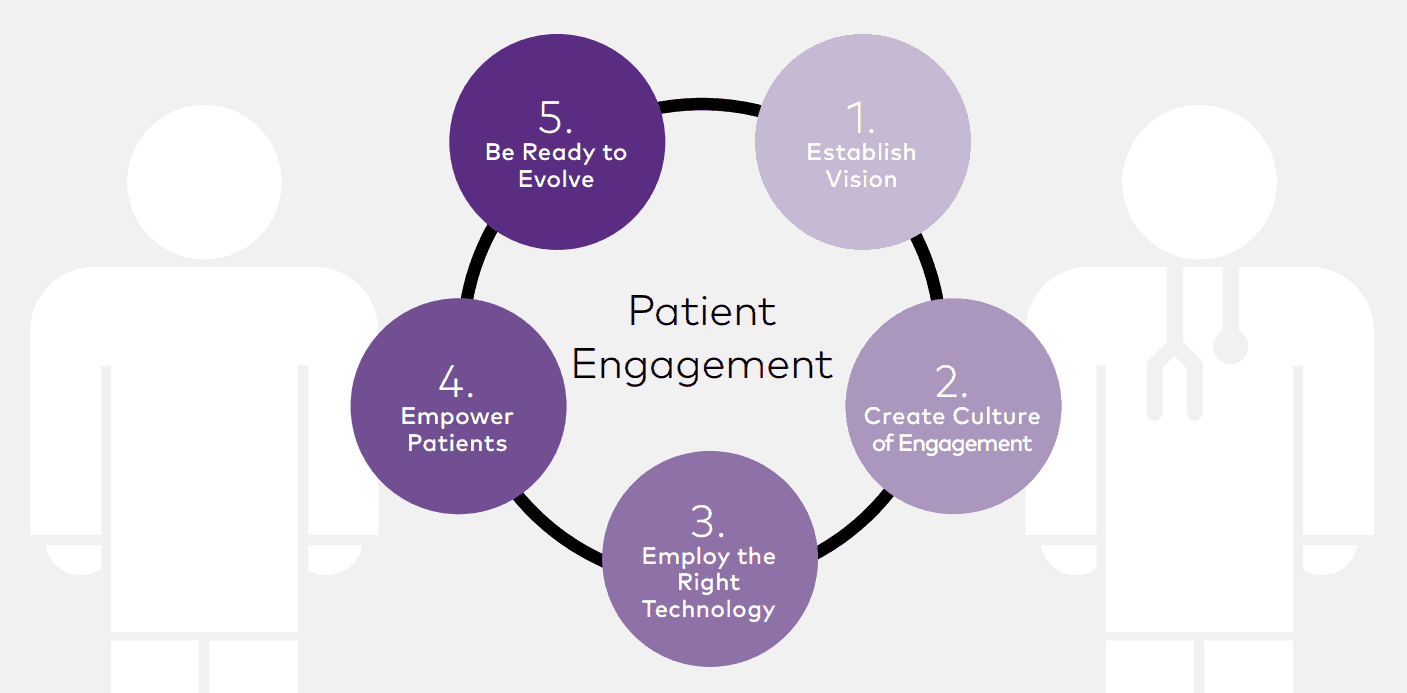
Dive Insight:
Patient engagement is a hot topic these days. During HIMSS17, a number of surveys made the rounds showing patients are using technology to engage with their health, though providers could do more to support the effort.
In the first half of 2017, digital health funding hit a record-breaking $3.5 billion on 188 deals, according to Rock Health. Patient engagement was one of the top categories, along with consumer health information, EHR/clinical workflow and analytics, and big data.
As organizations continue the move to value-based care, some hospitals and health systems are adding chief experience officers to the C-suite. In 2016, 44% of healthcare organizations reported having a CXO, and 39% of those reported directly to the president or CEO, according to a Vocera Communications survey.
8. Centralized Monitoring of Hospital Patients
Alarm fatigue is a top technology hazard in hospitals nationwide. The sounds that come from monitoring systems in hospitals can desensitize staff in critical situations after long periods of exposure. Nearly 44% of in-patient cardiac arrest cases are not attended to appropriately, and 90% of all alarms in hospitals aren’t actionable.
Centralized monitoring provides off-site monitoring of patients by technicians to give patients and clinicians the second set of eyes while providing better care from a distance. Technicians communicate directly with the caregivers on-site.

Using sensors and high-definition cameras, clinicians can monitor blood pressure, heart, respiratory rates, pulse oximetry, and more easily. An alert is generated that alerts caregivers on-site that help is needed. A recent study that evaluated the system reported a 93% survival rate of cardiopulmonary arrests using the systems.
9. LDL Cholesterol Drugs
There is a new class of LDL cholesterol-lowering drugs that are expected to be disruptors in the next year. The new drugs are expected to lower cholesterol to unprecedented levels.
When taken with a Statin cholesterol-lowering drug, the new class of drugs is expected to lower cholesterol levels by 75%.
The small interfering RNA therapy to lower LDL was also an innovation in 2017. They are given twice a year instead of monthly or weekly like other treatments.
Dr. Leslie Cho of the Heart & Vascular Institute at the Cleveland Clinic suggests that we will continue to see a new class of agents to lower LDL levels for years to come.
Statin drugs could one day be an over-the-counter drug, said Cho.
10. Gene Therapy for Inherited Retinal Diseases
Gene therapy for inherited retinal diseases is expected to receive a number of FDA approvals. Currently, there are no known treatments for the rare diseases, but the growing research of specific genetic etiology may soon restore vision loss in patients.

Recombinant AAV2 vector encoding a functional copy of the RPE65 gene is expected to receive FDA approval in the next year to treat retinal diseases that are caused by biallelic RPE65 mutations.
According to Dr. Aleksandra Rachitskaya of the Cleveland Clinic’s Cole Eye Institute, the gene therapy won’t cure blindness completely, but will instead preserve the vision that is already there. However, there are currently retinal implants out there that help cure blindness and researchers are using stem cell therapies to combat retinal diseases. She also said that a new methodology called optogenetics, which involved modifying cells to function as other cells, could bring new hope to treating the diseases.
11. Hybrid Closed-Loop Insulin Delivery System
The most anticipated healthcare technology disruptor will be the hybrid closed-loop insulin delivery system, better known as an artificial pancreas. It is the next step in creating a fully automated delivery system.
In 2016, the FDA approved the first hybrid closed-loop insulin delivery system. The system is designed to help manage Type 1 diabetes. It is a fully automated insulin delivery system that connects a continuous glucose monitor with an insulin pump, eliminating the need for people with diabetes having to test and manage their insulin levels themselves. Studies have shown that the system steadies blood glucose levels and has even dropped A1C levels by a half percent.
Jim Young, chair of the Endocrinology & Metabolism Institute at the Cleveland Clinic, said it’s not quite an “artificial pancreas” because it doesn’t perform all of the same functions of the Pancreas, but it does handle the insulin function well.
Young also suggests that it has taken so long to get to market because of a “fear of failure” – too much or too little insulin could be a problem.
An example is Medtronic, which had stepped ahead of the pack last September when it won FDA approval for its MiniMed 670G artificial pancreas hybrid closed-loop system, making it the 1st system of its kind to win clearance globally. While the system isn’t a stand-alone artificial pancreas, as it requires entry of carbohydrates and a baseline blood sample, it is a significant step toward the development of a fully capable closed-loop solution.

12. Non-Invasive Diabetes Monitoring
Apple is reportedly working on a “super-secret” medical project: building sensors to monitor blood sugar levels without piercing the skin and has hired a small team of biomedical engineers to work at a nondescript office in Palo Alto, California, miles from corporate headquarters.
They are part of a super-secret initiative, initially envisioned by the late Apple co-founder Steve Jobs, to develop sensors that can noninvasively and continuously monitor blood sugar levels to better treat diabetes, according to three people familiar with the matter.
Such a breakthrough would be a “holy grail” for life sciences. Many life sciences companies have tried and failed, as it’s highly challenging to track glucose levels accurately without piercing the skin.
More than 29 million people in the US suffer from diabetes, and many struggles to keep the condition in balance. “On average a lot of diabetes patients aren’t achieving what they want, and that’s all about their glucose control,” Jake Leach, senior VP of research and development at glucose monitoring system maker Dexcom, told us.
“So if we can provide them with better information to make better decisions on managing their diabetes, I think we can get some of these better outcomes that are going to ultimately reduce the cost of managing diabetes.”
13. 5G Mobile Technology
Fast communication and healthcare are not usually mentioned in the same sentence, but as wireless technology gets better, we are starting to see how the Internet of Medical Things (IoMT) will greatly improve patient lives.
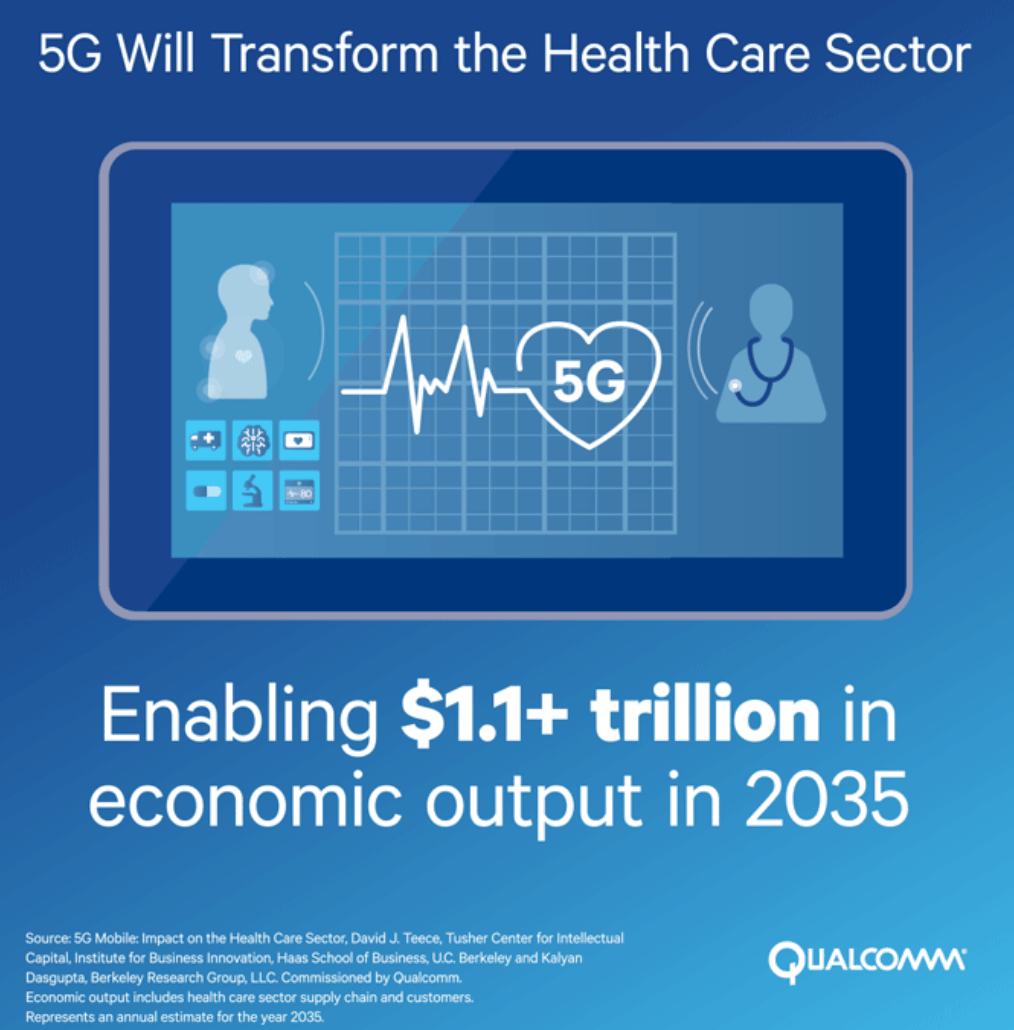
Qualcomm worked with Dr. David Teece, Professor at Haas School of Business, U.C. Berkeley, and Chairman and Principal Executive Officer of Berkeley Research Group, on a paper, “5G Mobile Impact on the Health Care Sector”. Qualcomm Technologies Inc. (QTI) commissioned this report to assess 5G’s potential impact on the evolving healthcare sector as it begins a shift in focus from volume-based health care to value-based (outcome-based) health care which could generate upwards of $650 billion in savings by 2025, according to Goldman Sachs.
5G enhanced Mobile BroadBand (eMBB) could save you a trip to the doctor.
If you don’t like visiting your doctor, that’s fine, because soon your doctor may visit you. Well, virtually that is. 5G is expected to usher in a new age of greatly enhanced eMBB data rates and hyper-connectivity, which will allow doctors to study and analyze numerous patient medical data feeds simultaneously and provide personalized treatment for patients.
Did we miss anything?
Interested in creating valuable content and sharing it with millions of our readers? Submit an application and join our healthcare technology blog.