Healthcare is a concern for everyone. With the continually changing industry, it’s important to acknowledge the different problems in different parts of the country. Rural and urban communities face different medical issues due to their location and their population numbers.
According to Medical News Today, geographical location affects the health of those living in it. This is partially due to the environmental differences that come from rural versus urban environments and access to medical care. Below are the benefits and challenges of both rural and urban healthcare and a combination of factors both communities face together.
Rural Medical Industries
Benefits of Rural Care:
Rural medical care offers a more personalized approach to healthcare for patients. Because most rural communities are close-knit, with small populations, doctors get to know their patients, families, and friends more easily. This type of care ensures a patient’s trust and increases the chances of a continuing and successful treatment program. In smaller populations, word of mouth can help keep a constant flow of patients and a good repertoire for rural doctors.
As a doctor, there is a perceived better quality of life in rural environments. Urban physicians may take home a higher salary, but the overall lower cost of living in a rural town can grant a more comfortable lifestyle for doctors. It allows them to purchase larger houses with more land, whereas there is more demand in the urban real estate market than housing supply. The price of urban homes is significantly more than the cost of rural homes.
Physicians who work in rural environments often have a better opportunity to expand their learning than their urban counterparts. Since rural doctors often take on cases they normally wouldn’t have seen in their medical courses or residencies, they become a “jack-of-all-trades-doctor.”
Due to a geographic lack of close resources like specialists and hospitals, rural physicians benefit from the wide variety of knowledge they have to assist patients with conditions that a specialist in a big city would typically treat. Medicine is often seen as a one-sided beneficial practice. A doctor treats a patient, and to their benefit, they get better. Or at least that is the way we hope it works. The truth is everyone benefits.
Challenges of Rural Care:
Rural communities inherently come with a smaller population and a smaller population of physicians per capita. Telemedicine has helped bridge this gap. Telemedicine is becoming more common because rural hospitals are closing (or haven’t even opened), and access to specialized care in rural areas is lacking. While it doesn’t replace a normal physician visit, an electronic meeting can help rural patients gain access to specialists without traveling great distances.
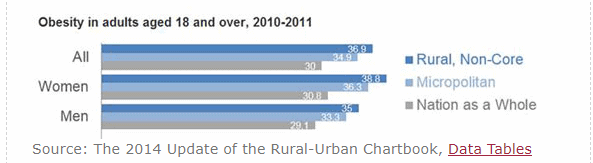
Obesity is a major concern for rural areas. While overweight issues often occur in rural and urban communities, children in rural areas experience higher obesity rates with less access to specialized care. Risk factors for obesity include poverty and a lack of access to healthcare, including obesity prevention and treatment services. They are less likely to have weight management experts, dietitians, or nutritionists available to help poor diet choices. Rural areas experience more cases of diabetes and coronary heart disease than non-rural areas. Poor food choices not only affect heart health but increases the risk of obesity as well.
An analysis done between 2007-2008 by the American Heart Association concluded that less than 1 percent of all American children met the diet guidelines for ideal heart health.
It was noted that eating habits were poor due to a lack of fruits and vegetables, lean protein, and whole grains. They found that kids were instead eating foods with high caloric values and low nutritional values. Since rural areas are typically poorer communities, they often lack money to purchase healthy food options.
Urban Medical Industries
Benefit Urban Industries
The medical benefits of an urban environment are probably the most understood of all the industries. By living and working in an urban environment, populations inherently have more access to different treatment options. Rural communities are often distanced from normal medical specialists, making their treatment more complicated.
Specialists are sometimes the saving grace when it comes to health complications. Primary physicians are trained to spot many medical issues, but they do not always have the knowledge to understand underlying issues and concerns with a complicated ailment. Urban patients benefit from the additional knowledge and counseling they get from doctors practicing there. Specialists are more accessible to these patients, which helps deal with complicated issues in a more effective and timely way.
On the flip side, a higher population leads to an increased need for doctors. This allows for more job stability and more options for employment for physicians. As a doctor, urban communities offer many medical issues and concerns that create a consistent need for treatment and job stability. Unlike rural communities, this close access to healthcare means that patients are more likely to continue and complete necessary treatments. This keeps a consistent patient population available to practicing physicians.
Challenges Urban Industries
Urban careers as a whole have increasingly become more stagnant, which is far different from rural neighborhoods. James Levine concluded in 2005 that any extended period of sitting could be harmful. He went as far as to say that sitting was the “disease of our time.” Physical inactivity can cause anxiety, depression, increased risk of cancer, cardiovascular disease, coronary heart disease, decreased muscle mass, high blood pressure, and elevated cholesterol levels. In fact, according to the World Health Organization, more than 80 percent of the world’s adolescents were physically inactive.
According to the CDC, adults should aim for 150-300 minutes of exercise weekly. This can be a combination of aerobics, cardio, or low-impact yoga. Some specific urban factors discourage people from being more active, like a fear of crime in outdoor areas, low air quality, and a lack of community infrastructures like parks, recreation facilities, and sidewalks. These concerns and deficits in the community can affect a person’s desire to work out regularly.
It is not a secret that our urban communities are growing more than anticipated. Crowded living conditions in big cities correlate with high transmission of infectious diseases. Since the population is closer together than it would be in rural communities, it allows for diseases and viruses to shift from person to person quicker. The NCBI says that chronic diseases and acute diseases have been linked to respiratory issues in urban populations. With the increase of pollution complication issues in urban environments, chronic respiratory infections are on the rise. Infections like SARS and the avian flu have the potential to spread quickly in highly populated areas.
An unfortunate downside to crowded living conditions is the creation of urban slums. Since there is a population in poverty in large cities, these economic issues create problems for the urban medical industry. Fast urbanization brings way to slums and, subsequently, poor hygiene conditions. Infectious diseases spread through contaminated water, which is often the only water available. A lack of access to clean water makes it difficult for some families to carry out basic hygiene functions. Half of the urban populations in Africa, Asia, and Latin America are still suffering from diseases and infections due to a lack of access to sanitation and safe drinking water.
Overlapping Challenges in Rural and Urban Healthcare
Vaccine hesitation is becoming a major issue amongst all facets of healthcare. Parents are the primary cause of vaccine hesitation in both rural and urban environments. Their three major reasons for rejecting vaccinations in their children are:
- They think vaccines are no longer needed because the diseases are gone.
- They fear that vaccines are associated with adverse reactions.
- They think that they should be able to decide what medically happens to their children.
While parental concerns should be taken into account, the truth is, this vaccine hesitation epidemic has led to an increase of infections in children. In January 2015, a measles outbreak in California happened. At the time, 3.1 percent of kindergartners had nonmedical exemptions from getting the Measles Mumps Rubella (MMR) vaccine. Forty-five percent of the students who did not receive a measles vaccine or had an unknown vaccination status were affected. This outbreak spread beyond California boards, touching multiple states for many months. The argument that some parents have about diseases being gone is now null. The true reason that diseases have slowed in their exposure is that of these vaccinations and their protection.

Photo by Luis Melendez on Unsplash
A shortage of healthcare workers has urban and rural medical facilities scrambling to keep up with incoming medical issues. The most recent projection estimates that we are more than likely to see a deficit of 40,800 and 104,900 doctors in 2018. The report focuses on the healthcare workers shortage in four broad categories: medical specialists, surgical doctors, primary care physicians, and other specialists.
By 2030 it is estimated that there will be a deficit of 7,300-43,100 primary care doctors. Specialists will account for a shortage of 35,000-61,000 in 2030. The same report notes that by 2030, the number of Americans 65 years or older will grow by 55 percent. This will make the projected deficit of doctors even more significant. As patients grow older, they require two to three times as many services. More specifically, the growing older population will face a shortage of specialists.
Addiction-Specific Challenges
The opioid epidemic in our country has reached far beyond rural and urban borders to affect every facet of our population. According to the CDC, opioid overdoses accounted for more than 33,000 deaths in 2015 and 56,000 in 2016. According to NCBI, the United States holds only 5 percent of the world’s population but consumes over 80 percent of the world’s opioids. With numbers this staggering, there is no denying it anymore: prescription drug abuse and addiction have reached epidemic proportions.
Addiction typically begins with a legitimate injury or pain that is then rectified by a dosage of painkillers provided by a physician. Once the patient has used the prescribed medications, they are often unintentionally addicted to the substances. When their supply ultimately diminishes, they begin controlling their withdrawal symptoms with a cheaper street opiate like heroin.
The opioid addiction problem came together in tandem with the rise of over-prescribing prescription painkillers, as well as a high possibility of abuse. Due to specific jobs prevalent in rural cities like farming and manufacturing, these communities tend to have high injury rates. This leads to more pain and, in turn, more medication. Opioids have been a key part of rural doctors’ pain management tools for their patients.
On the flip side, urban careers require a lot of sedentary time. This alone, as mentioned previously, can lead to a whole host of complications. These can lead to nerve pain, a decrease in muscle mass, etc. These complications from an urban lifestyle can lead to an increased need for pain medication.
Conclusion:
The medical industry can vary widely from community to community. The important thing to remember is that it is constantly changing and improving. Thanks to advancements in technology, patients have more access in rural areas to specialists than they probably ever did. The level of care a patient receives should not be dependent on their geographical location as it is today. With acknowledgment of the issues surrounding rural and urban healthcare, there are sure to be changes made to better everyone in the future.