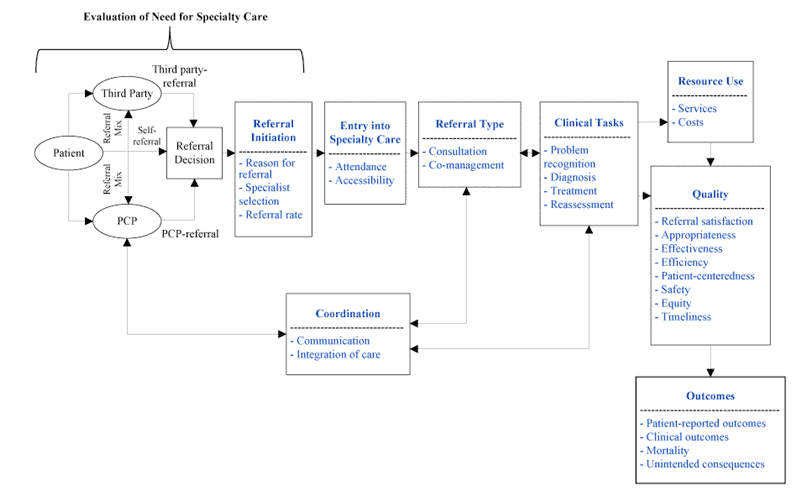
 Primary Care Physicians look to specialists for referrals to gain additional insights, and order laboratory tests, or imaging studies. The variation in referral use and management is dependent upon several scenarios. Specifics include patient characteristics, practice size, health plans with gatekeeping arrangements, as well as the variation of practices with managed care (Forrest, 2006).
Primary Care Physicians look to specialists for referrals to gain additional insights, and order laboratory tests, or imaging studies. The variation in referral use and management is dependent upon several scenarios. Specifics include patient characteristics, practice size, health plans with gatekeeping arrangements, as well as the variation of practices with managed care (Forrest, 2006).
The dissimilarity leads to the high cost of referral management and communication, un-uniform patient care, the inability to track referral needs as well as inaccurate data collection.
Primary Care to Specialist Referral Process:
Problem with the current referral system:
The referral and authorization process per insurance plan is complex and labor intensive for the providers and the payers. Each plan has its unique requirements for the providers to submit information and access the plan. Since there are multiple insurance plans with a variety of benefits, it is increasingly more difficult to manage the process in a streamlined and cost-effective manner.
Managed care transactions require an enormous amount of paperwork, especially when the referral requests and authorizations never catch up to the claims submitted for the already provided services. This results in a delay in payment to the provider and resubmitted claims as well as phone calls to the plan to resolve the problem. Because the system is so fragmented and contracts and coverage for members are changing it is extremely difficult to stay current with the requirements on a daily basis.
Reimbursement is declining, and costs are increasing for getting authorizations and receiving payment for services from the health plans. Healthcare is known for being labor intensive, but a majority of those costs are not associated with direct patient care but for administrative costs associated with the system of coordinating the services of authorized care.
This requires meeting all the insurance plans requirements for each of their members, and then they will provide payment. Cash flow is a significant issue for providers today, and delays in reimbursement for submitted claims needs to be addressed because of the overall negative impact on the hospitals, physicians, payers and the patients requiring services.
Shocking statistics
-
-
- It costs nearly $250 billion to process 30 billion healthcare transactions each year 1
- The average ratio of staff handling the paperwork to doctors can be as high as 8:1 1
- 86% of mistakes made in the healthcare industry are administrative 3
- Three of every ten tests are reordered because results cannot be found 4
- Patient charts cannot be found on 30% of visits 5
- Providers need to fill out an average of 20,000 forms every year 6
- Organizations, on average, make 9-11 copies of each document, spend $20 in labor to file each document and lose one of every 20 documents 7
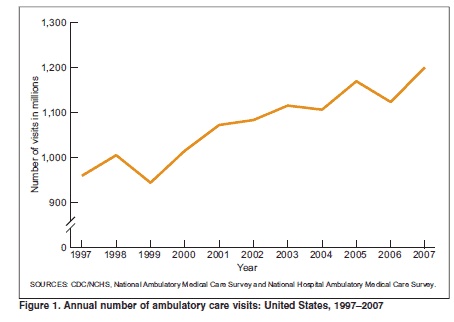
- Annual Number of Ambulatory care visits (1.2 to 1.3 Billion) 8
- 15 billion faxes are still sent by US physicians per year 9
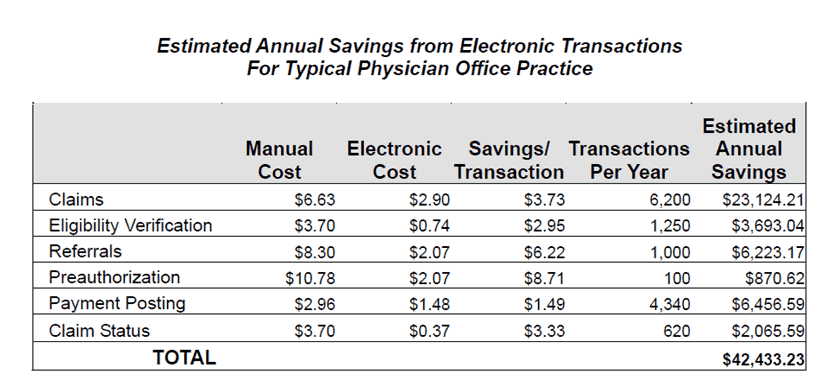
- To quantify the savings achievable per physician, Milliman10 estimated the annual transaction volumes of a typical solo physician practice and then estimated the cost to perform these transactions manually and electronically. The annual cost for manual transactions was over $70,000; the annual cost for electronic transactions was less than $28,000. Subtracting the annual electronic cost from the annual manual cost resulted in savings of over $42,000 per year from implementation electronic transactions, as indicated in the following table.
- Each misfiled document costs $125. 11
- According to a 2009 report in the health policy journal, Health Affairs, when the time is converted to dollars, physicians, nurses and their clerical staff spends between $21 billion to $31 billion per year interacting with insurance plans, inquiring about prior authorizations, formularies, claims, contracts and other patient information. The same article noted medical assistants earn an average of $30,000 per year, so essentially a medical practice is paying $12,000 a year per worker to talk to health plans. 12
-
So what does all this mean?
An average small practice can save $1,000’s a year (much more for a large healthcare facility) by updating to a standalone (agnostic) referral system such as ReferralMD. But this is not the main benefit, the reduction of errors and the ability to capture many more referrals as revenue are much more important.
Not only is the time a factor, but a very high percentage of paper referrals are either physically lost by the patient or by the facility thus incurring a huge liability to both the primary care and specialist provider. Every patient referral that is lost or misplaced can affect patient care quality and cause a direct reputation hit on the facility.
Think about this the next time you send a 1-way fax communication.
Sources:
1 Woodworth, Glenn. “2003: The Year of Medical Paperwork Simplification,” Journal of Healthcare Information Management Winter 2003, vol. 17. no. 1, pp. 12-13.
3 Woodworth , Glenn, “2003: The Year of Medical Paperwork Simplification,” Journal of Healthcare Information Management
4,5,6 “A Healthy System,” Technology CEO Council, 2007
7 Pricewaterhouse Coopers
11 http://www.thepaperlessproject.com/what-are-the-facts-about-paper/
12http://tinyurl.com/aqg4mnm
8 http://www.cdc.gov/nchs/fastats/docvisit.htm
9 Marketsandmarkets, July 2, 2012
10 http://tinyurl.com/bgzjtxu