It’s no secret that nurses work hard. The layperson would shudder at the long shifts most medical staff experience, but nurses take it on without blinking. They continually administer medications, check-in with families, advocate for their patients, and work with a medical team for the best results possible within a convoluted medical system. In stories from across the country, nurses share days where they don’t get a lunch break, have patients on gurneys in hallways, and are jumping from department to department to make up for staffing shortages. The bottom line, there is (or will be) a nursing shortage. How do we solve the problem?
About The Nursing Shortage
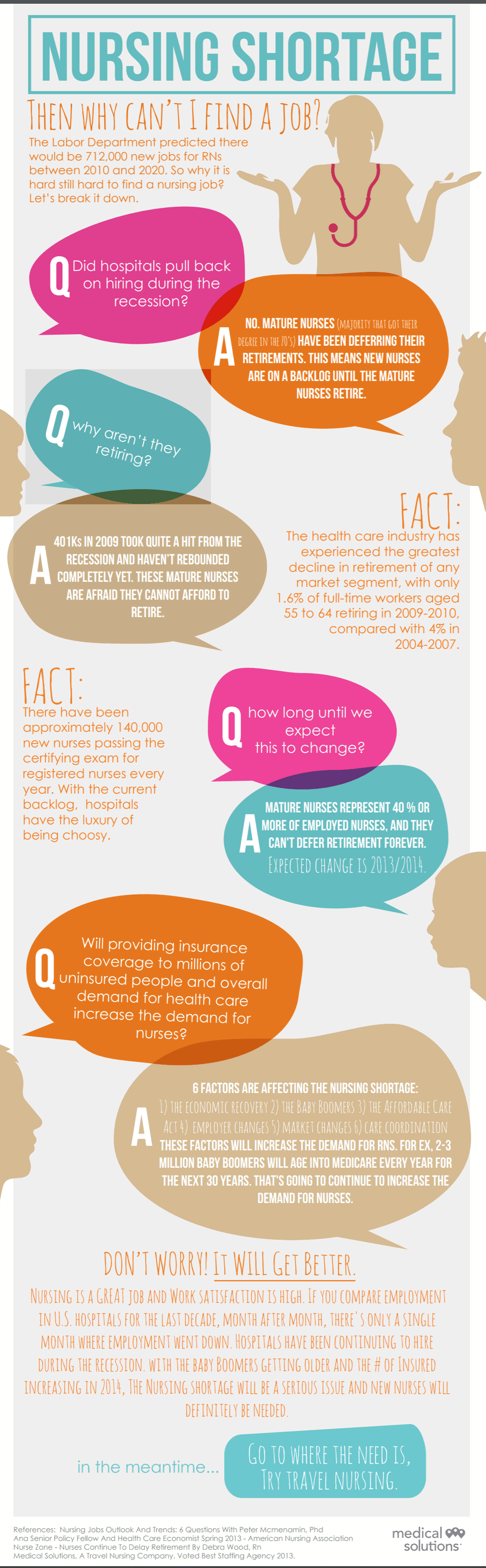
The United States has a massive nursing shortage, and the problem is only set to grow. Due to an influx of patients into our health system, the retirement of baby boomers, and educational bottlenecks, nursing positions aren’t being filled fast enough to keep up with demand. While on the surface it may seem like a simple supply-and-demand equation, the actual cause and projected effect is much more complicated. Without intervention on multiple levels, the problem will not go away.

Who Is the Nursing Shortage Impacting?
Obviously, the burden of a nursing shortage impacts those nurses who are working in the field. As more nurses retire or change careers and fewer nurses enter the field, the work is piled higher on those left working.
When the Affordable Care Act was passed, it gave more Americans access to healthcare services and consequently increased the number of patients seeking care. According to Bradley University, 92 percent of emergency rooms report patient overcrowding. That translates to increased wait times for patients, but it also means more evaluations for nurses and higher pressure to treat patients efficiently.
Short-handed nurses under pressure are at a higher risk of making mistakes. A study performed in Denmark found that readmission rates rose as nursing staff diminished, indicating that patients were discharged prematurely or not treated entirely before being sent home. The study further noted that patients in nursing homes, where the draw of nursing employment is not as strong as in hospitals or clinics, saw an astonishing 13 percent increase in the mortality rate of older patients.
Patients obviously suffer when nurses feel the time-constraining effects of understaffing. As our population continues to age, the prognosis looks grim: more than 80 percent of adults over 65 have at least one chronic condition. More than 65 percent have two. With baby boomers continuing to age, the percent of the population requiring regular care will continue to put pressure on healthcare practitioners.
Doctors are seeing the strain as well. Insurance companies and hospitals create an impossible equilibrium where doctors must decrease the amount of time they spend with patients in order to maintain a profitable bottom line. Nurses feel the strain as more of the workload is transferred to them, as well as picking up any pertinent missing pieces of patient health history that may not have been disclosed to the doctor.
The nursing shortage also has financial impacts on healthcare institutions. Nurses’ salaries must be competitive to attract applicants. As the shortage fuels burnout and frustration among nurses, turnover rates increase, reportedly costing the healthcare industry at least $4.2 million a year.
Why Is There a Nursing Shortage?
While practitioners, patients, and institutions illustrate that there is an undoubted need for nurses, it’s not for lack of interest. Prospective nurses looking to enter the field encounter a gauntlet of obstacles that make filling the healthcare need that much more difficult.
Educational Obstacles
Students appear to have a high level of interest in nursing careers. They pay well, have strong projected job security, and allow practitioners to do meaningful work — all qualities that millennials have expressed are important.
However, as hopeful applicants send in their transcripts, many are turned away or wait-listed. Some schools have even done away with waitlisting due to excessive demand that has students waiting years before their enrollment.
One of the major limiting factors in nursing education is low faculty numbers — there simply aren’t enough teachers to educate the would-be nurses. Not only that, but the current faculty’s median age is in the 50s, meaning that many of them will be looking to retire not long from now.
It’s difficult to draw more faculty to schools, as taking a teaching position requires a nurse to have a higher level of education, be an expert in their field, and often, be willing to take a pay cut. For some of the larger schools, providing enough financial incentive to leave a clinical position and move to teach may be feasible, but for smaller, private, or rural institutions, the financial burden may be too much. Without nurse educators in rural or underserved areas, we are further limiting the accessibility of nursing school to potential students.
Another issue contributing to the bottleneck in nursing education is the lack of clinical sites available. Without hands-on experience, nurses are entering the field lacking a critical understanding of what running codes and assessing patients is like. Hypotheticals cannot replace the stress of how life-and-death decisions feel in real-time. Without more clinical learning positions available, nursing programs will not be able to increase the number of applicants they accept.
Financial Obstacles
For those who are accepted into nursing programs, there’s something more to contend with: the cost of schooling. Whether trying to attain a nursing license through an associate, bachelor’s, or master’s program, the costs add up. And on top of it all, those pursuing a specialty have to be prepared to devote years to their professional development. RNs pursuing an oncology specialty, for example, not only have to earn the degree, but they also have to invest years of time and money into board certifications and clinical practice hours. It all adds up.
Grants and scholarships like the RN to BSN/MSN Challenge can help with this burden, but unfortunately, there just aren’t enough to go around. Title VIII of the Public Health and Service Act is a federal program that awards grant money to nurses working in underserved regions.
Peter McMenamin, a former American Nurses Association representative, stated to Healthline, “There’s a direct correlation between Title VIII funding and new nurses.” The article continues on to discuss a bill that would extend grant and loan funding through 2020. Unfortunately, that bill was introduced in 2015 and was passed by the House of Representatives, but not by the Senate.

A similar bill, H.R. 959, was introduced to the House on February 10, 2017, and would extend federal funding through 2022. The bill has not yet gone to vote. If it passes the House and the Senate, federal funding will be extended and enrollment in nursing programs will hopefully see an uptick.
While fingers get crossed for the extension of funding, two other bills stand to undermine some of the financial cushioning for nursing school graduates.
The new tax bill still needs to be reconciled between the versions the House and the Senate each passed, but depending on which way the hand of fate swings, public service loan forgiveness may be eliminated. If the House tax plan is honored, graduate students face higher interest rates and elimination of student loan interest deductions. Employer-provided tuition assistance would become a taxable benefit, placing an additional burden on employees seeking higher education.
The PROSPER Act (Promoting Real Opportunity, Success and Prosperity Through Education Reform) was proposed in early December and has yet to go to vote, but it has serious implications for those with student loans. Most notably for nurses, Public Service Loan Forgiveness would be eliminated. For those who carry substantial debt, loan forgiveness might be the only light at the end of a 10-year tunnel. Moving forward, repayment options would shrink from eight separate plans to two, severely limiting the options of borrowers.
Workplace Obstacles
Part of paying back loans, especially if a nurse is attempting to be eligible for Public Service Loan Forgiveness, is maintaining employment. With the nursing shortage, it shouldn’t seem like a problem. However, while there may be a plethora of positions available, that doesn’t mean all the positions are optimized for retention.
Some things are basic: paying nurses enough and making sure they have the tools to do their job. While many programs are offering signing bonuses and generous salaries to increase hiring during the shortage, the effects of fewer staff members are felt throughout hospitals and clinics.
Fewer nurses mean that the ones who are employed experience a higher workload, and often have to cover shifts or work overtime to keep patients covered. The combination of higher pressure and more hours worked can lead to staff burnout, both emotionally and physically.
Compassion fatigue can affect caregivers who aren’t able to take time for themselves or who are too stressed in their work environment. Minimal sleep from picking up extra shifts, combined with the emotional energy required to care for additional patients, can contribute to burnout and inadvertently cause the quality of patient care to decline.
Quality of patient care is also impacted by the experience of the nurses — seasoned veterans of the career will be calmer during codes, understand the procedure better, and have a more developed sense of what patients need. While experienced nurses are able to pass along some of this knowledge, more baby boomer nurses are retiring than ever.
AMN Healthcare’s survey found that 73 percent of older nurses intend to retire in the next 3 years. That leaves patients with a much younger, less experienced staff who are seeking mentorship as they get their feet under them. The high retirement number not only contributes to the nursing shortage but also to the stress and working conditions of those left in the workforce. Those who don’t intend to retire immediately face the daunting task of bringing new nurses up to speed on how individual programs run and giving them the day-to-day tips and tricks to make it as a nurse.
Despite being new to the field, nurses may change career paths within a few years, citing workplace bullying or other stressful conditions as their reason. In some cases, nurses are faced with ethical dilemmas or matters of practitioner autonomy that they feel inhibit their ability to treat within the best interest of their patients — 75 percent of nurses report feeling like they don’t have enough authority. When situations like this arise and are not addressed satisfactorily, nurses may leave programs feeling like they are unable to fulfill their duties.
Minimizing the Nurse Shortage
There’s a lot of work to be done if the U.S. is to effectively mitigate the nursing shortage. Policy, both at the federal and institutional level, stands to play a large role in the change. In some cases, attitude or expectation shifts may be necessary. What are the trends?
Program Growth
Primarily, the US needs to increase the number of potential nurses in educational programs, as this will directly impact the number of nurses available to enter the workforce. It is estimated that by 2025, the workforce will need more than half a million new nurses, which in turn means that programs need to provide openings for as many applicants.

Educational opportunities will only grow with the addition of funding and faculty, though the first does impact the second. Universities need to reassess their programs and see where they can afford to increase salaries in order to attract faculty. Non-monetary incentives, such as access to campus resources or publishing connections, will also be necessary to retain top teaching staff.
From a federal perspective, the government needs to increase Title VIII funding and retain the possibility of Public Service Loan Forgiveness. The elimination of either program will hamstring an already struggling effort and create an even larger practitioner deficit. Making grants and funding available to those from impoverished or rural areas will create a larger pool of talent to draw from.
Hands-On Training
Before entering the field, nurses need experience making stressful decisions in real-time. Many teaching hospitals and healthcare education programs are turning to technology for answers. Using simulation mannequins, computer programs, or virtual reality situations allows educators to put nurses in controlled situations to test their knowledge under pressure.
Simulation technology may be the best answer to creating more opportunities for field training new nurses without taking time or energy from practicing nurses. Virtual situations allow nurses to make mistakes without the high-stakes environment of having a patient’s health in their hands.
Where possible, the availability of clinical rotations needs to increase. Hands-on training is essential for up-and-coming nurses, and the current number of opportunities is far too low. Care facilities will need to update programs to allow for shadowing and teaching.
Experienced nurses may find the addition of observers to be a hindrance to their daily tasks, but until more nurses are trained in a hands-on way, there will not be more competent, comfortable nurses coming to lighten the load. In conjunction with asking experienced nurses to devote even more time and energy to their professions, facilities need to improve the quality of life available to their staff.

Quality of Life Improvements
While many articles remind nurses of how to cope with stress and fatigue using healthy strategies, advice like “get adequate sleep” and “take breaks while at work” can be frustrating if schedules don’t allow for it. Rather than asking nurses to do what feels impossible within their circumstances, employers need to accommodate their nurses’ basic needs and listen to their feedback.
Several programs across the country provide examples of doing just that. Funded by grant money, nursing programs are turning inward to invest in their nurses and find out what needs to happen to reduce turnover and keep happier staff. In one instance, a program retained 95 percent of the charge nurses who participated in a program to help develop their own resources.
Competitive pay, flexible schedules, and plentiful training resources will aid programs in retaining and developing their nursing staff, as well as drawing new hires. As retention increases, facilities will lose less money through turnover and be able to focus their financial resources in other areas that need improvement.
Immigrant Nurses
As a temporary solution, the United State may look towards hiring nurses from other countries. Currently, foreign nurses make up approximately 15 percent of the workforce. While foreign nurses may dull the growing pains in the short term, it’s only a temporary fix — the United States will still be responsible for systemic overhauls to internally mitigate the situation.
Nurses attempting to work in the US may be frustrated by the visa process, as H1-B visas can be complicated to obtain. Working with the government to ensure the success of their prospective employees can cost facilities time and money. During this time, immigrants may opt to settle in a different country with a simpler process.
Once set to work, American hospitals still have to contend with quality of life and retention issues among their foreign hires. Many nurses are still unhappy with the working conditions in the United States and will make attempts to leave before their contract is up.
Looking Forward
Clearly, neither the blame nor the burden of repair lies in any one place. In order to combat the effects of the United State’s nursing shortage, healthcare facilities will need to work with newcomers and veteran nurses to develop effective training solutions. Combined with supportive government measures and funding, the future of patient care faces a reduced mortality rate and a happier workforce.













