Photo by OpenClipart-Vectors on Pixabay

Photo by OpenClipart-Vectors on Pixabay
In the most basic sense, patient access refers to the ability of patients and their families to take charge of their own health care. With the advent of the internet and digital marketing, medical practices and health clinics have a new way to reach their target audiences. This has slowly empowered patients to take control of where and when they receive their medical care. With review sites like Healthgrades and ZocDoc, patients can now read and leave reviews about doctors, nurses, staff, health centers, hospitals, etc.
Choosing your provider and your place of care is almost like picking a restaurant for dinner! (read the reviews) However, patient access means different things to different entities. For example, hospitals view patient access in terms of their “patient access department.” These branches are responsible for every patient that walks through those hospital doors.
They make sure that all newcomers are properly registered, that their insurance is verified, and at the end of their care, that they are billed appropriately. Health strategists and policy experts tend to define patient access as all of the things that affect a patient’s ability to receive the proper care at the proper time and proper place.
What Does This Mean for the Healthcare Practice or System?
This means that patient access is indicative of how effective the health center is as-a-whole. It refers to all operational aspects of the business – the doctors, the nurses, the staff, the facilities, the IT, scheduling, and even coordination amongst referring providers. All of this adds up to a care experience that will either be beneficial or a hindrance to your patient access program. i.e. customer service.
For example, implementing an online scheduling platform (checkout ReferralMD’s solution) can be a very effective method to improve patient access. Prospective patients can easily go on a provider’s website and book an appointment that fits both their and the provider’s schedules.
However, if the practice fails to meet patient needs in other aspects of care such as lack of providers, inconvenient business hours, or unsuitable geographic location, then having an online scheduling platform is of no real benefit to that health organization. As a result, patient access management can be considered a combination of all that a health center offers in terms of the care it provides to patients.
What Happens When Patient Access Goes Wrong?
An example of patient access gone wrong can be seen in the 2014 Veterans Health Administration Scandal. During this period, patients at VA hospitals were not being seen within the target time of 14 days. Some of these patients died while they were waiting for an appointment. The most extreme case was in Phoenix where 35 veterans died while waiting for care (Source).
Now, there were a number of problems with the VA hospitals that allowed for something like this to happen. Mainly, these hospitals were heavily understaffed and held to unrealistic standards. The existing staff and schedulers were pressured into making wait times more favorable through unethical practices such as falsified appointment records. This led to more than 120,000 veterans waiting for or never even receiving care (Source).
Patients waiting for or not receiving care is one of the major problems associated with patient access. The following step-by-step guide will help your health system avoid situations like this and maximize patient access.
How to Improve Patient Access
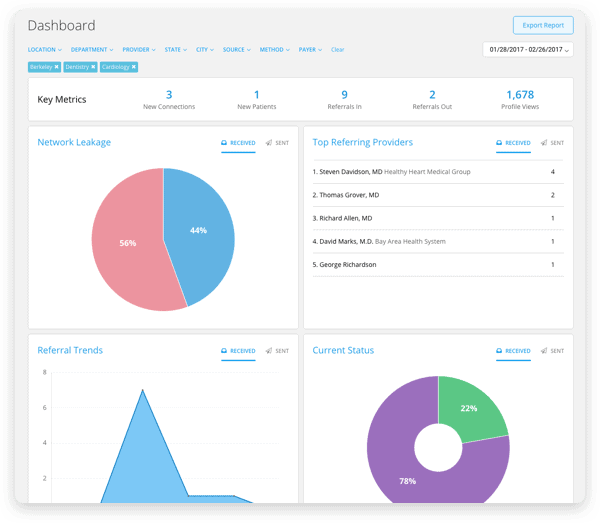
Step 1: Measure and Monitor Access and Workflow
The first step for any health organization/system should be to implement a method of monitoring and measuring patient access and patient workflow. This means that you should know how long on average a patient must wait before they can get an appointment at your facility/facilities. For smaller practices, you can do this by making a monthly log and recording available appointments as they appear.
After gathering a month’s worth of data, you can look at the data points and see the variation between appointment availability. It is important also to monitor the number of cancellations, no-shows, reschedulings, and appointment denials that your practice experiences. Most health businesses and systems can do this in their current EHR software, but others need a more robust platform that can offer detailed analytics and real-time updates on patient care.
Try ReferralMD’s industry-leading referral management solution today for free! It helps to streamline the referral process, improves communication amongst providers, and reduces wait times for patients.
Click here to get started
Once you have appointment data, you are better able to adjust your operations so that you maximize appointments and scheduling for patients. Another thing to measure and monitor would be the actual workflow within your place of care. By measuring the time it takes patients to go through certain steps of the medical visit, you can see where potential bottlenecks exist and where improvements can be made. This can easily be done by having one of the staff manually record and log the time it takes for patients to go from point A to point B to point C, etc. within the continuum of care.
Step 2: Have an Organizational Meeting to Discuss Potential Solutions
The next step after gathering both access and workflow data is to gather your staff and providers for an organizational meeting. During this meeting, you should share and discuss all of your findings from Step 1, and then come up with organizational strategies and ideas to address these issues. Your staff should provide reasons for why appointments are not being scheduled or are being missed.
For example, the patient may only want to see a certain provider who may be booked or may not be available (out of town, on vacation, etc.). In some cases, it could be the staff’s fault. Patients may be complaining that they need to see the doctor immediately. However, the receptionist or scheduler is not trained to know whether certain complaints are severe or not. These are all patient access issues, and therefore, you and your staff must come up with solutions to fix these problems.
Here are some ideas to fix patient scheduling issues:
-
- Provide receptionists and schedulers with a list of symptoms via the SmartMATCH Decision Support technology so they can direct patients to the appropriate care.
-
Schedule immediate appointments for patients with complicated symptoms or conditions.
-
- Implement a policy to refer patients with basic symptoms to a physician assistant (PA) or nurse practitioner. It is not necessary for them to see a doctor or specialist.
-
- Hire part-time nurses, PAs, or providers.
-
- Invest in an open-access scheduling software or platform to put scheduling in the patient’s hands using ReferralMD’s patient access tools.
With ReferralMD’s scheduling widget, you can easily post a link to the top of your website allowing prospective patients easy access to schedule their own appointment according to availability within your calendar.
Step 3: Implement an Action Plan
Now that you and your staff have discussed potential solutions, it is time to implement an action plan so that you move forward with actually addressing the patient access issues at hand. Depending on the solutions that you and your team have come up with, it is important to lay out the following:
-
- Description of each solution
- Description of each solution
-
- Realistic timeline to implement and accomplish each solution
-
- Resources required for each step
-
- Who is in charge of what
There should be someone in charge of each solution so that multiple things can be accomplished within the same time frame. In addition, there should be one person (the office manager for example) that oversees the entire project to ensure that everyone and everything is in order. For each solution, outline all the steps necessary to accomplish the task and then assign each task to a person. Have them record their progress along the way, from beginning to end. They should also take note of any potential roadblocks as well as if they need additional assistance or more resources. Let’s look at an example: Say you and your staff have decided to introduce an open-access scheduling system to allow patients to schedule their own appointments on your website. There are a number of steps that are required before you can follow through with this.
-
Outline metrics that will allow you to determine if the system is successful.
-
- Reduces the number of patient rescheduling, no-shows, cancellations, etc. by half
-
- Saves your staff an average of 10 hours/week
-
- Improves patient reviews on sites like Zocdoc or Healthgrades
-
-
Determine what features you would like and how much you are willing to pay for the system.
-
- Features – scheduling system, patient portal, scheduling widget, etc.
-
- Develop a cost-benefit analysis or a risk profile to decide what price is appropriate. (Learn more about that here and here, respectively.)
-
-
Evaluate different vendors.
-
- Do your due diligence to find the appropriate vendor for you.
-
- Does your EMR software already offer this service? If so, it may be easier to implement through them.
-
- Create a vendor profile and weigh the pros and cons of each system to what you are looking for (outlined in Step 2.)
-
-
Decide on a vendor and move forward with implementation.
-
- Make sure the website is up to date and is compatible with the scheduling system.
-
- Implement system.
-
- Notify patients of the new system through blast email or phone call (can automate to make easier – separate step)
-
-
Measure progress and record success of the system
-
- Determine if the system is successful based on metrics outlined in Step 1. (make sure to give it some time – say two months, to see if the system is working)
-
As you can see, this is a detailed outline of what goes into implementing a solution. You should be doing this for every strategy that you come up with in order to determine whether it will be successful or not.
Step 4: Measure and Monitor Results to See What Works and What Doesn’t
The final step with any of your potential solutions is to evaluate. It is vital to measure and monitor the progress of each of the strategies that you have implemented. The whole goal here is to improve patient access to your health system. Therefore, you should be evaluating each of the programs to ensure that it is having a tangible positive effect on access. There are a number of ways to go about monitoring results:
-
- You and your staff can do it manually, measuring and recording the improvement in appointment access or operational workflow, or use the ReferralMD Analytics Solution. This can be done by monitoring the variation in appointment cancellations and rescheduling amongst your patients. Operational workflow can be measured by timing patient visits and comparing them to previous metrics.
-
- You can have someone monitor patient reviews online to see if patients are leaving positive feedback. The hope is that improving access leads to the improved overall care and improved patient satisfaction.
-
- You can create and send out surveys to all of your patients asking for feedback on new solutions such as open-access scheduling or part-time providers. You can create these in SurveyMonkey easily.
-
- Measure the number of basic symptom cases that are no longer being seen by the doctors/providers and are now being addressed by the nurses/physician assistants. This frees up more appointments for the doctors eventually resulting in more complicated cases being seen by them.

Photo by mohamed_hassan on Pixabay
In conclusion, there are many ways to go about improving patient access in your healthcare system. It’s all about taking initiative and being structured in your approach.