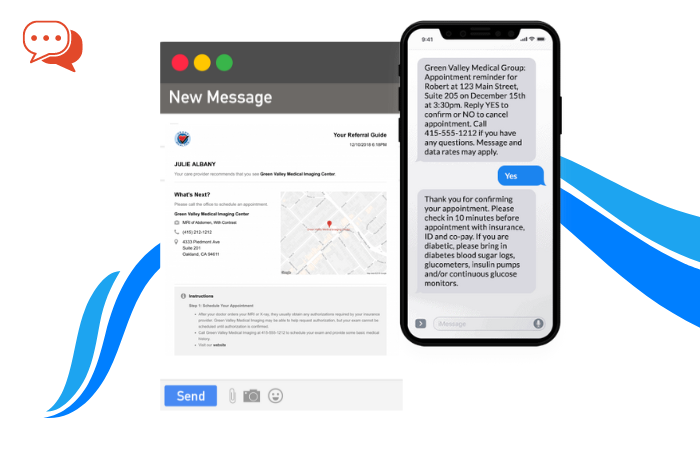
Patients want quick and timely solutions. And they may choose a service that offers essential treatments and looks into their behavioral health.
Effective primary care is all about providing ease and convenience to the patient. It helps them achieve better health more efficiently. You can think about integrating behavioral health with primary care.
Why? Doing so will improve the sustainability of practices, making it more convenient for the patients. Generally, these practices involve a fee for service (FFS) or value-based care payments (VBC).
Behavioral health and primary care services need smart planning. If done intelligently, they can impact the patients’ lives immediately.
In this post, we will look into some ways you can sustain behavioral health in primary patient care. But before that, find out what behavioral health is.

Photo by Emma Simpson on Unsplash
What is Behavioral Health
Behavioral health encircles the emotional aspect and behaviors that affect a person’s well-being. At times, behavioral health is referred to as mental health too. But it’s more sophisticated than you might think.
Just like you have a family doctor for your physical health, there are trained physicians. And it generally involves substance use.
Interestingly, mental and behavioral health care are co-dependent at times. Patients with mental health issues exhibit unhealthy habits. These habits define their entire behavioral health and are the causes of such illness.
If you have bad behavioral health, it can trigger mental illnesses. Some bad behavior health indicators include:
- Drinking
- Overeating
- Drug abuse
They can lead to mental complications.
How to Merge Behavioral Health in Primary Care
Primary care experts recommend some tried and tested methods for sustainable behavioral health. Most of them stressed giving sustainable solutions. According to them, sustainability should be on top of the list when designing a behavioral health process.
Here are some key methods to enhance sustainability with behavioral health in primary care.
1. Making it Feasible
Adding behavioral health to primary care is a great way to enhance monthly revenue for the healthcare sector. It does not depend on the number of patients a healthcare service gets. The revenue may increase because they will charge separately for behavioral health.
From the available data, it was evident that PHQ9, AUDIT, and GAD7 screenings were billed for patients with behavioral health issues. Moreover, integrating the two sectors helped increase the number of encounters with the patient.
As a result, there was more revenue, but more importantly, it improved the outcomes for the patients.
2. Associated Protection
When you’re looking for a ‘primary care doctor near me, one of your objectives could be to receive the ultimate patient care at one location. Sustainability encompasses all areas, including:
- Psychological well-being
- Physical health
- Mental health
Because of the integration of behavioral health with primary care;
- There is an element of associated protection
- Patients feel at much ease
This combination ensures that patients receive the due care from one place. Patients tend to prefer hospitals where they can receive all types of services under one roof. This prevents complications during their treatment.
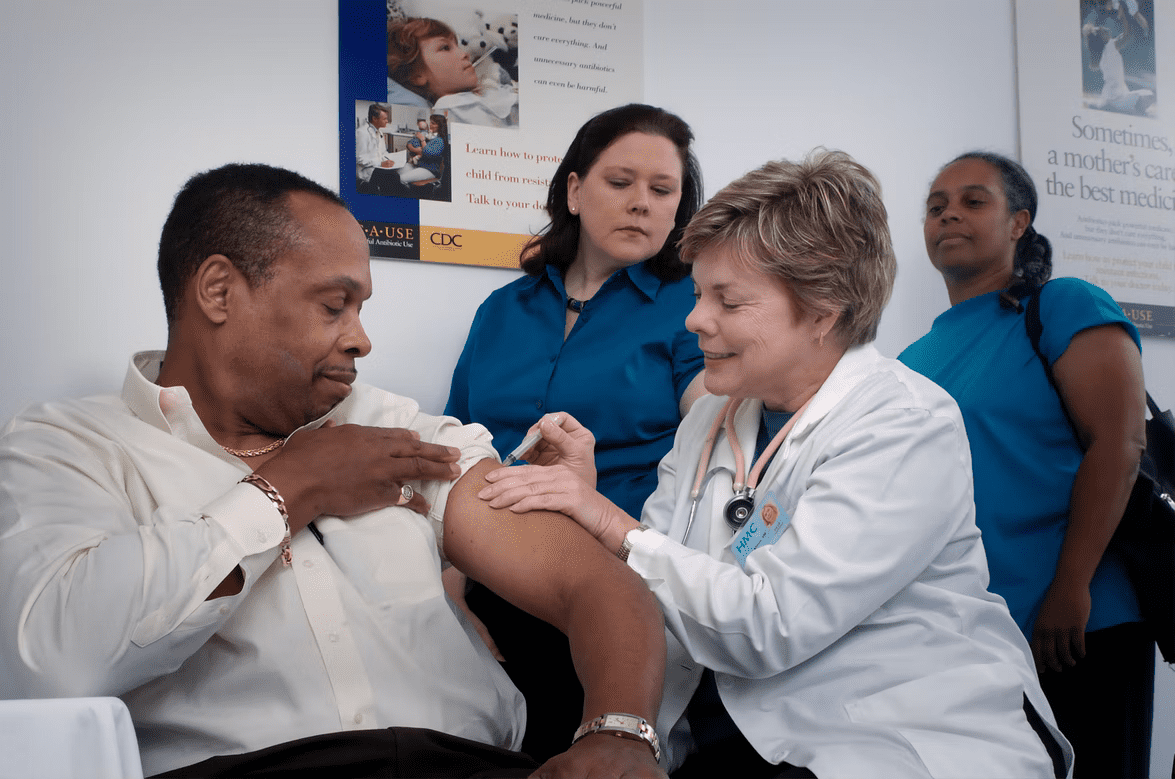
Image source: Unsplash
3. Preparing for Monetary Success
The role of management is quite critical when it comes to an integrated care system. So, there is a need to wear at least two thinking caps:
- A primary care doctor
- An active management personnel
In addition, when healthcare setups are preparing for monetary success, the planning must be robust. Here’s what they can do to ensure well-defined workflows and proper planning:
- Healthcare managers must be active participants in planning with those involved in billing.
- They need to have (or follow) business models from the Current Procedural Terminology.
A well-managed healthcare unit has more chances of engaging patients who have different needs. So, when patients need a professional specialized in a specific field, they know where to go.
4. Anticipating Your Billing from Integrations
Dr. Henry Chung is a renowned Professor of Medical Psychiatry in the Albert Einstein Faculty of Drugs. He is also the VP of the Care Administration Group of Montefiore Medical Center in New York.
Dr. Henry emphasizes that healthcare setups must anticipate different types of billing. It must support various levels of integration between behavioral health and primary care.
According to his analogy, healthcare institutes can work efficiently with the following framework:
Preliminary
This model is limited to screening and treatment. Moreover, services supported by grants may also be billed under this model.
Intermediate Level I
It involves billing for screening and treatment services. These services may include:
- BH treatment
- PHQ screening
- Care coordination
It all lies under fee for service, and the providers must have efficient mechanisms for the reimbursement processes.
Intermediate Level II
At this level, healthcare institutes charge a service fee for quality incentives. They are directly related to behavioral health integration with primary care practices.
Advanced
It involves global payment receipts. It focuses on the achievement of behavioral health and other general health outcomes.
Benefits of a Behavioral health Model
Integrating behavioral health into primary care can yield substantial results for healthcare institutions. The results of such integrations show how they helped patients to improve their depression scores. At the same time, they must enhance the overall patient and physician experience.
Several medical studies also suggest that integration can help reduce the monetary burden on the patients. How?
They have access to an integrated model-based healthcare system to get mental health solutions. Because of this flexibility, they are less likely to visit emergency services. In general, it means better overall health for the patient at a reduced cost.
These integrated models have been applied to many hospitals across the globe. Although there is room for improvement, the results have been quite positive.
Here are some noticeable results:
- Improved financial position
- More investment in research and development
- More robust solutions for primary treatments
- Increased level of trust and satisfaction from patients
Conclusion
When used smartly, integrating behavioral health and primary care can be a lucrative model for healthcare setups. For patients, getting immediate care services becomes more manageable. Health services featuring integrated models can engage such patients more readily.