Accurate information for personalized, value based care
In a world where value-based care is prioritized, healthcare providers ACOs, FQHCs, Healthcare Systems, and Hospitals must comprehensively understand a patient’s health to effectively manage costs, mitigate risks, and deliver high-quality, personalized care. A key aspect of achieving these goals is ensuring that the patient’s health conditions are accurately and wholly coded, as this plays a crucial role in determining appropriate payment for the care delivered and the sharing of associated risks.
Value based care is essential for healthcare providers for several reasons, as it represents a shift from the traditional fee-for-service model to a more patient-centric and outcomes-focused approach. Here are some key reasons why value-based care is essential:
- Focus on Patient Outcomes:
- Value-based care emphasizes achieving positive patient health outcomes rather than simply providing services. Healthcare providers are incentivized to deliver high-quality care that leads to better patient outcomes, which can result in improved patient satisfaction and overall health.
- Cost Efficiency:
- By emphasizing preventive care and efficient management of chronic conditions, value-based care aims to reduce unnecessary healthcare costs. Providers are motivated to deliver care cost-effectively, which can lead to better resource utilization and overall cost savings.
- Quality Improvement:
- The quality of healthcare services is a central focus in value-based care models. Providers are encouraged to adopt evidence-based practices and follow clinical guidelines to ensure patients receive the most effective and appropriate care. This can lead to improved overall healthcare quality.
- Patient Engagement:
- Value-based care encourages greater patient engagement and shared decision-making. Patients become more involved in their healthcare decisions, leading to better adherence to treatment plans, improved communication with healthcare providers, and, ultimately, better health outcomes.
- Population Health Management:
- Value-based care promotes population health management, which involves addressing the health needs of entire patient populations. Providers are incentivized to implement strategies for preventive care, early intervention, and managing the health of whole communities, leading to improved overall health at a population level.
- Reduced Fragmentation:
- Value-based care encourages better coordination and communication among healthcare providers. This reduces the fragmentation of care, where patients may receive disjointed or duplicated services. Care coordination can lead to a more seamless and integrated patient healthcare experience.
- Payment Reform:
- Value-based care involves a shift away from fee-for-service reimbursement models toward alternative payment models that reward providers for delivering high-quality, cost-effective care. This change in payment structures aligns financial incentives with positive health outcomes.
- Adaptation to Changing Demographics:
- As the population ages and the prevalence of chronic conditions increases, value-based care provides a framework for managing these complex healthcare needs more effectively. It encourages proactive and personalized approaches to care delivery.
- Regulatory and Payer Emphasis:
- Many healthcare regulations and payer initiatives support the transition to value-based care. Providers participating in value-based care programs may benefit from financial incentives, regulatory compliance, and enhanced relationships with payers.

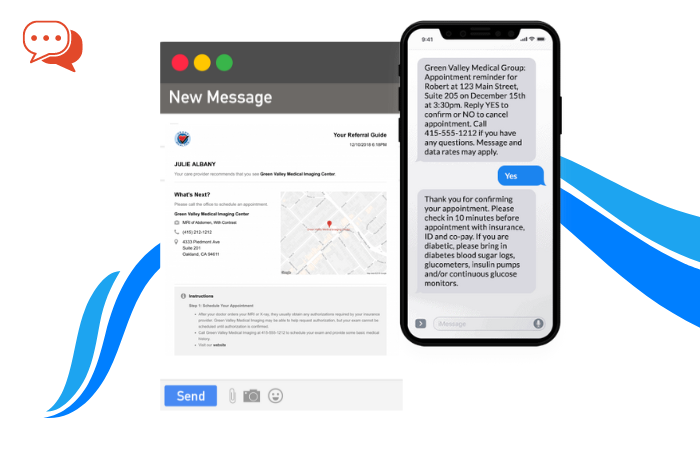
ReferralMD offers a robust solution that allows healthcare providers and payers to track the complete life cycle of a referral. By utilizing ReferralMD, healthcare organizations can exchange data in real-time with all community providers, regardless of the Electronic Medical Record (EMR) system they use. This seamless data exchange ensures that critical patient information is readily available to all relevant parties involved in the patient’s care.
With ReferralMD, providers can capture and document pertinent clinical information during the referral process, ensuring that the patient’s complete health history is accurately recorded and shared. This comprehensive data sharing facilitates better care coordination, improving patient outcomes and enhancing collaboration among healthcare professionals.
Additionally, ReferralMD streamlines the payment and reimbursement process by ensuring that accurate coding of the patient’s health conditions is captured. This enables appropriate payment for the care provided and allows risk-sharing arrangements to be accurately implemented.
By leveraging ReferralMD, healthcare organizations can effectively manage the complexities of value-based care. They can optimize the exchange of information, coordinate care more efficiently, and ensure accurate reimbursement. Ultimately, ReferralMD empowers providers to deliver personalized, high-quality care while managing costs and minimizing risks.
In summary, value-based care is essential for healthcare providers because it promotes better patient outcomes, cost efficiency, and quality improvement. It aligns healthcare delivery to keep populations healthy rather than solely focusing on treating illnesses reactively. This approach is seen as a more sustainable and effective way to address the evolving challenges in the healthcare landscape.