Research shows that 93% of patients prefer to use technology when communicating with medical practices. Yet, 61% of health insurance claims are denied due to errors originating in patient intake forms. This disconnect highlights a critical gap in healthcare administration—one that modern intake and scheduling solutions are well-positioned to address.
Automated intake software can save medical assistants up to 30 minutes a day and reduce documentation time by 45%. Patients also benefit, as they can complete forms from home with greater accuracy and convenience. To maximize these benefits, practices need a solution tailored to their specific workflows and patient populations. This guide will walk you through the process of selecting and implementing the optimal patient intake and scheduling system for your organization.
Assessing Your Practice’s Automation Needs
You need a clear picture of your practice’s specific challenges before implementing any patient intake solution. The path to successful automation begins with a comprehensive understanding of your current workflows, staff activities, and patient experiences.
Identifying current workflow bottlenecks
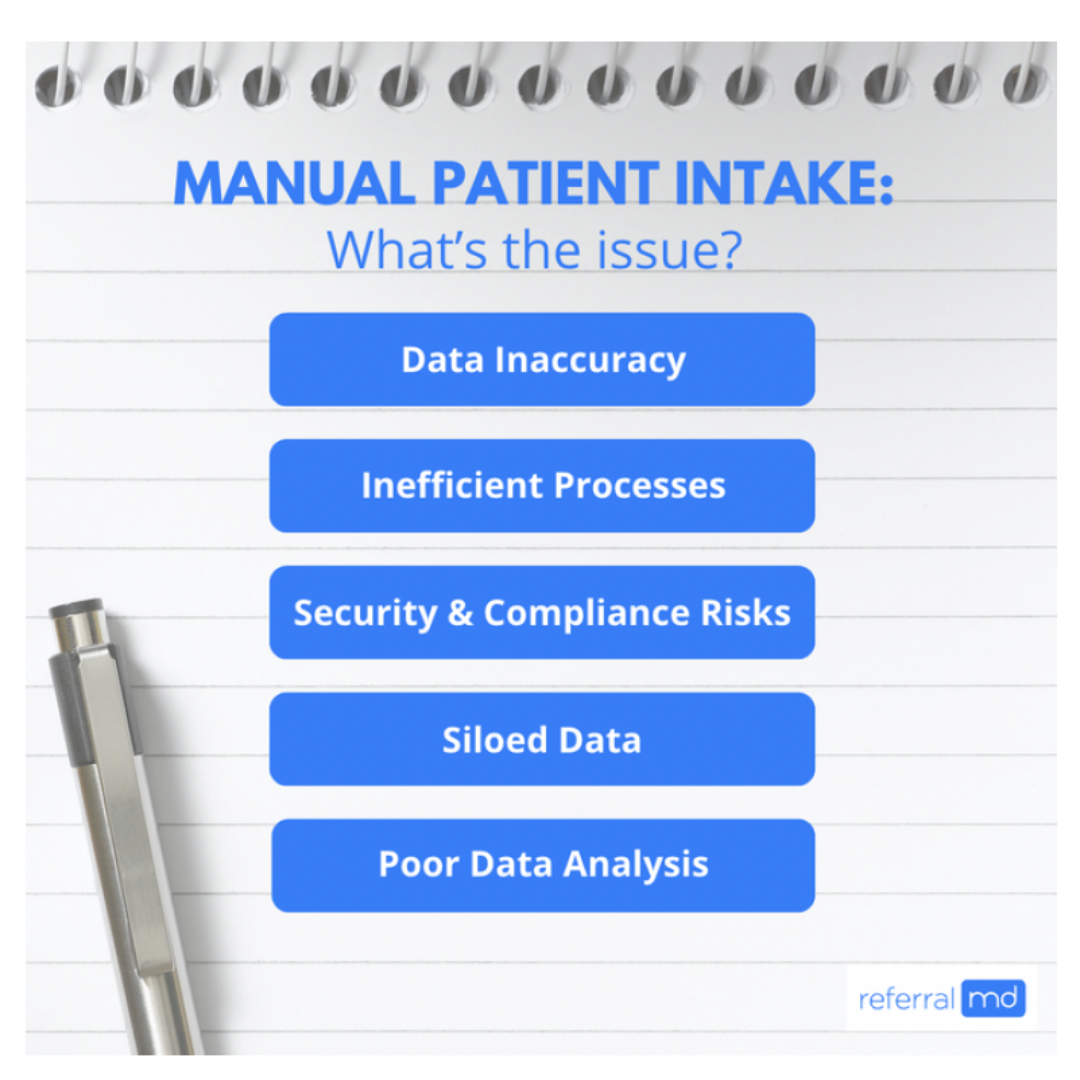
Resources that can’t handle patient volume create bottlenecks in healthcare settings. These bottlenecks slow down care processes. Paper forms and manual data entry in traditional patient intake often result in significant slowdowns. Staff frustration grows and your practice’s bottom line takes a hit because of these inefficiencies.
Start by mapping your current intake workflow from start to finish to identify these bottlenecks. Write down each step and note where delays usually happen. Ensure that you document which systems are connected to your most significant problems. A single system change can alleviate multiple pain points simultaneously. This detailed analysis helps you focus your automation efforts where they will make the most significant difference.
Evaluating staff time spent on manual tasks
Healthcare staff spend about 37% of their time doing administrative work and desk duties. They spend just 9-22% of their time with patients. Nurses also spend a significant amount of time working with electronic health records (21.51 minutes) and completing paperwork (31.63 minutes) during observed periods.
Manual data entry creates one of the biggest time drains. Your staff must type all patient information into your EHR or practice management system when using paper forms. This double work often leads to mistakes that can be costly when claims are denied.
Your team might work more efficiently if you spot tasks they could delegate or automate. Studies show that nurses could use about 10% of their time more effectively if they didn’t have to perform tasks that others could handle. Track how many hours your team spends on paperwork versus patient care to determine where automation would provide the most benefit.
Traditional Intake Pain Points
Patients don’t hide their frustrations with traditional intake methods. Research shows 75% of patients would rather fill out forms digitally than use paper. This preference makes sense given the problems they face.
Patients hate waiting in your office. Check-in delays from paper forms mess up your appointment schedule and create longer wait times. Unhappy patients often result from these delays. Rushed patients usually fail to provide complete information on paper forms, resulting in incomplete records.
Patient privacy creates another primary concern. Paper forms containing sensitive information are not secure, which increases the risk of HIPAA violations. Understanding these issues helps you select intake management software that addresses your practice’s most pressing problems.
Home-Based Convenience & Renovation Integration
As more patients engage with healthcare from home, intake automation supports a smoother experience even before they leave the house. Patients can complete digital forms from their devices, upload insurance documents via smartphone, and receive appointment confirmations through voice assistants or smart home hubs.
For patients, seniors, and individuals with mobility challenges, digital health tools provide an essential bridge to care, enabling regular communication with providers without the burden of frequent office visits. Automated patient intake simplifies the healthcare experience by offering seamless digital check-ins, medication updates, and appointment management from the comfort of home. Caregivers also benefit from gaining an easier way to support their loved ones’ healthcare needs through intuitive, tech-enabled solutions that prioritize accessibility, convenience, and improved health outcomes.
Selecting the Right Patient Intake Management Software
Your practice needs the right patient intake management software. You should assess several essential factors to find a solution that matches your specific needs. The best software will optimize your workflow and improve patients’ experience.
Key features of effective patient intake solutions
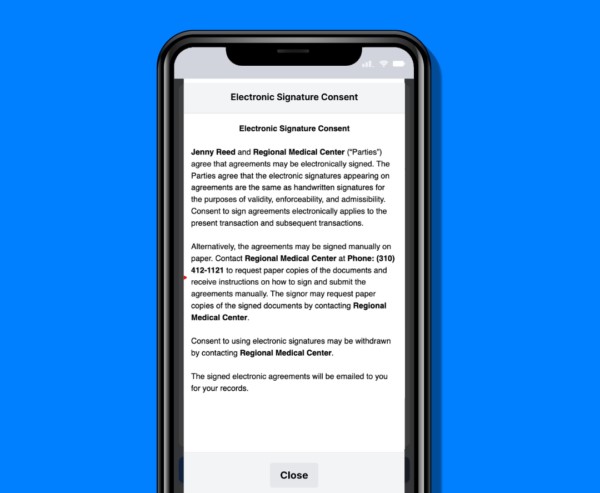
The best patient intake solutions automatically fill registration forms by pulling data from ID and insurance cards. Live validation features spot and correct data entry errors immediately, ensuring information remains accurate and consistent. You’ll want systems that let you customize forms without coding or waiting for vendor changes. Patient data protection is vital, so your solution must comply with HIPAA rules, utilizing strong encryption and user verification.
Modern healthcare is increasingly leveraging smart technology to enhance patient engagement and care management. Voice-activated assistants, connected health devices, and automated intake systems collaborate to provide a seamless healthcare experience at home. Patients can receive appointment reminders, complete digital pre-visit questionnaires, and securely share vital health data with providers—all from familiar, tech-enabled devices. By integrating these innovations into daily life, healthcare organizations can empower patients, streamline workflows, and support better outcomes across the continuum of care.
Comparing cloud-based vs. on-premise options
Cloud systems run on remote servers with a subscription model that includes automatic updates and room to grow. Your team can access patient records from any internet-connected device, which helps optimize clinical workflows. Cloud options cost less upfront but need ongoing subscription payments.
On-premise software resides on your local servers, granting you complete control over your system and customization. You’ll spend more money upfront on hardware and software licenses, but this might save you money over time by avoiding subscriptions. Small practices might struggle with this option because it requires in-house IT staff for updates and maintenance.
Integration capabilities with existing EHR systems
Your new system must integrate seamlessly with your current Electronic Health Record (EHR) setup. Look for solutions with two-way integration that can read and write to your practice management system. Third-party options often offer more flexibility for customization. The system should utilize interoperability standards, such as HL7 and FHIR, to facilitate data exchange.
Budget considerations and ROI potential
Software licenses, better hardware, and integration services make up your original costs. You can spread these expenses over time with a step-by-step implementation plan. Track your ROI through staff time savings and reduced claim denials resulting from improved data accuracy. While measuring ROI requires effort, automating repetitive tasks typically yields clear efficiency improvements.
Implementation Strategies for Successful Adoption
A new patient intake solution needs strategic planning to ensure your organization adopts it smoothly. Your users will accept the system more readily and achieve improved long-term outcomes with a thoughtful implementation approach, rather than rushing the deployment.
Creating a phased rollout plan
Successful implementations work best with a phased approach instead of a “big bang” deployment. Research shows that phased rollouts minimize business disruptions while allowing you to verify that you’re heading in the right direction. Your original plan should start with the least disruptive changes. More substantial modifications can be gradually layered on top of smaller ones. Your staff can adjust to small changes over several months, rather than undergoing a single massive transition.
Staff members need a “test mode” that they can use in each phase to understand the platform fully. You’ll have control over when changes go live, and your team will feel more confident throughout the implementation process.
Staff training and change management
The implementation of new technology depends on effective change management. The core team should champion the new patient intake management software to aid peer-to-peer learning. Different roles require tailored training sessions designed specifically to meet their needs.
A complete training program helps address resistance by including:
- Hands-on practice in simulated environments
- Continuous support through help desks and super-users
- Regular measurement of effectiveness with adjustments based on feedback
Research reveals that psychological concerns and fears of increased workload often hinder the adoption of digital technology. Your training program should address these concerns early to facilitate easier adoption.
Patient education on new digital tools
Patients should know about upcoming changes before implementation begins. Studies reveal that 92% of patients prefer completing pre-visit questionnaires online rather than by phone or in person. Patients appreciate knowing how your intake solution saves time, eliminates redundant data entry, and reduces in-office wait times.
Healthcare organizations typically send educational materials through text or email. Patients learn about the tool right after scheduling an appointment. Good education helps patients value the convenience and improved service your practice provides.
Measuring Success Through Performance Metrics
Your patient intake management system requires specific performance metrics to assess its effectiveness and identify areas for improvement. The success of what you implement can be measured through carefully picked KPIs in several regions.
Time-saving KPIs
Patient intake automation brings quick benefits in efficiency. Our customers report that their office staff work more efficiently with fewer manual tasks. Here are the key things to measure:
- Patient throughput – Track the number of patients processed per period
- Check-in time reduction – Compare average check-in times before and after implementation
- Administrative time saved – Measure reduction in staff time spent on paperwork
Medical assistants save about 30 minutes each day thanks to optimized processes.
Error reduction measurements
Digital intake forms help reduce documentation errors. Manual administrative errors account for 86% of healthcare mistakes, making it crucial to track and improve accuracy. Monitor fewer errors in medication dosing, prescription writing, and insurance claims. The data should be more reliable and consistent than your old manual methods.
Patient satisfaction indicators
These metrics indicate the effectiveness of your system. Research reveals 90% of patients would rather fill out pre-visit questionnaires online. Digital patient experience surveys sent via email, text, and QR codes increase response rates by 23%. The Net Promoter Score (NPS) and satisfaction ratings should be checked regularly during different care stages to obtain a comprehensive picture.
Financial impact assessment
The money saved often makes automation a worthwhile investment. Consider metrics such as time-of-service collections and reduced claim denials. Healthcare workflow automation saves money – research shows the U.S. healthcare system could save $16.3 billion through more transaction automation. Compare your setup costs against ongoing efficiency gains to measure both quick savings and long-term ROI.
Conclusion
Patient intake automation proves to be a game-changer for modern healthcare practices that need better efficiency and accuracy. Healthcare practices can streamline their intake processes and reduce administrative work by conducting proper evaluations, implementing solutions effectively, and tracking results.
The numbers tell a compelling story. Medical assistants save 30 minutes each day, while documentation time falls by 45%. Patients show a clear preference for digital solutions. These improvements enhance both operational efficiency and patient satisfaction.
The path to success begins with selecting the right software that meets your practice’s specific needs. You need a measured implementation approach and regular performance monitoring. Don’t call it a one-time project – this is an ongoing experience toward excellence in practice management.
Healthcare practices that adopt digital transformation will see patient intake automation deliver real results. Staff productivity soars, errors decrease, patient satisfaction improves, and financial performance improves. A comprehensive understanding of your needs helps build strong foundations for lasting, positive change.