If you have met me personally, I have been known to cuss a few times in my life, not as much as Dave McClure from 500 startups though. If you have been under a rock lately then you may have not read our PART 1 version of the “11 Reasons Why” post that went viral in the healthcare community.
It has been shared 1000’s of times and commented on in groups such as the Healthcare Executive Network on LinkedIn, which is boasting 83,000 + members.

Click the image to view the 200 plus comments
What inspired me to write the first post was that I was fed up with the current system and wanted to share my opinions with the world. I had no idea that it would spread as far and as fast as it did.
So after a short break from the original article I decided to create my next opinion addressing another 11 reasons why healthcare is completely broken.
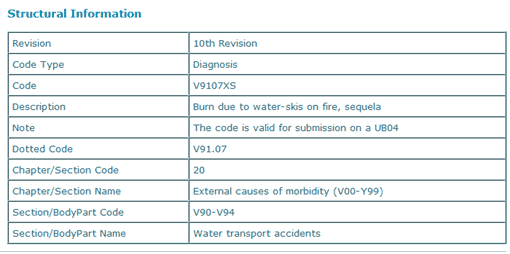
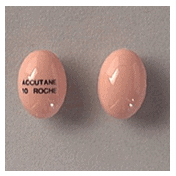
ICD-10
A code for everything!
All I can say is “Really?”,
The US Department of Health and Human Services (HHS) has mandated the replacement of the ICD-9-CM code sets used by medical coders and billers to report health care diagnoses and procedures with ICD-10 codes, effective Oct. 1, 2014. ICD-10 implementation will radically change the way coding is currently done and will require a significant effort to implement.
Now comes the funny part
There is literally a code for almost everything, don’t believe me?
 SITUATION: You’ve been involved in a water-skiing accident where your skis have caught fire and now you are being rushed to the emergency room.
SITUATION: You’ve been involved in a water-skiing accident where your skis have caught fire and now you are being rushed to the emergency room.
I really wish I was kidding, but I am not.
THE GOOD NEWS: There a code for that. ICD-10-CM, (“we have to pass the bill so that you can find out what is in it”) has anticipated this and your hospital will have no problem billing insurance for your treatment.
THE BAD NEWS: There are 6 different codes for this situation and you’ll be delayed as the medical administrator has to choose one.
More funny codes:
Z3754 Sextuplets, all liveborn
W5922xS Struck by turtle, sequela
Z62891 Sibling rivalry
Z631 Problems in relationship with in-laws
V9107xD Burn due to water-skis on fire, subsequent encounter
T505x6A Under-dosing of appetite depressants, initial encounter
V616xxD Passenger in heavy transport vehicle injured in collision with pedal cycle in traffic accident, subsequent encounter
V9733xD Sucked into jet engine, subsequent encounter
T63442S Toxic effect of venom of bees, intentional self-harm, sequela
Z621 Parental over-protection
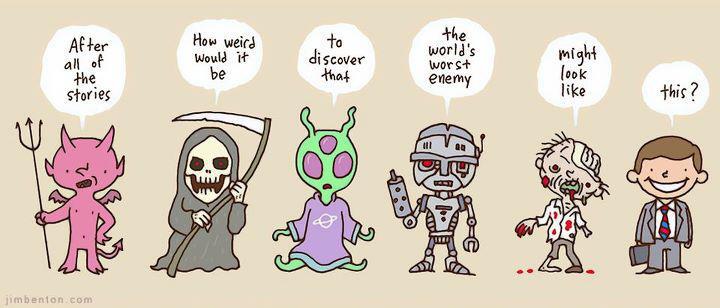
Prescription drugs:
Over-prescribed and the side effects
Doctors are rewarded for prescribing drugs. Big pharmaceutical companies are known to hand out “consulting agreements” worth more than your annual salary to doctors who prescribe their drugs like candy. … This is one of the worst practices I can think of that drives a stake right through the heart of healthcare’s credibility
And unfortunately it seems people take accept it and take pills for everything.
Have a headache? Take a pill. A rash? Take a pill. Sore muscle? Take a pill. Tired? Take a pill. Overwhelmed? Take a pill. The list goes on and on.
- Why do people these days feel the need to take a pill for every ache and pain they have?
- What do they think people did before these medications were around?
- Why are doctors so easy to prescribe a pill for everything?
- Is it an easy way out?
- Are they getting paid from the drug companies to prescribe them?
Ugly (and disturbing) Truth to side-effects
 Drug: Alli
Drug: Alli
Used For: Weight-loss/Weight-control.
Obesity has reached record-highs in this species of ours, and there are many who would quite literally do–or endure–almost anything, just to go down 1 dress-size. However, as many know, there is almost always a catch. And the catch for Alli takes the cake (no pun intended). Side effects range from uncontrollable bowel movements, to loose stools, to…”oily spotting”. Naturally, this “oily-spotting” is accompanied by flatulence. The website for Alli describes the “oily-spotting” as such:
“…You may recognize it as something that looks like the oil on top of a pizza…”
That sure is a lovely image. And the website states this side effect as a “minor” problem. However, this problem can be solved by limiting or entirely stopping your fat intake. Which raises the question:
Why even take Alli in the first place?? Why not just remove fat from your diet?
 Drug: Accutane
Drug: Accutane
Used For: Acne
Having pimples is no fun, we all have them from time to time, but to go to an extreme and take a pill that has the side effects that cause crying spells, rectal bleeding, and bone fractures (oh my!) is absurd.
I think I would rather have a few zits.
Somewhat less amusing, and well worth the description of “alarming” are side effects like hepatitis, psychosis and hirsutism. That last one is, in fact, an overabundance of hair. Finally, and we’re unsure of the logistics on this one, but according to Rxlist.com, you can also, somehow, end up with herpes.
Basically, in your quest to get rid of acne, it’s not outside the realm of possibility, slim though it may be, that you could end up as a psychotic wolfman with VD. One with anal bleeding.
Healthcare Lobbying:
AARP : A non-profit that is for profit.
A wolf in sheep’s clothing, drinking the blood of trusting souls that do not know any better.
This may be a strong statement but look at the facts.
- AARP’s haul from sponsoring insurance plans have nearly tripled in recent years to $657 million a year.
- Former CEO Bill Novelli got a raise of more than 80 percent from 2007 to 2009 even as the recession was taking hold. Novelli’s pay went from a little over $900,000 a year to more than $1.6 million.
- Some of the money also goes to lobbying — AARP is the fourth highest-spending lobbying group in Washington with other healthcare related companies following suite (AMA, Pharma, AHA, Blue Cross/ Blue Shield )
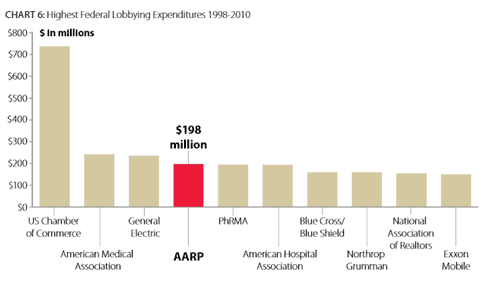
Making the Big Bucks!
As the facts set forth in this report reveal, AARP is not simply a non-profit entity claiming to advocate on behalf of America’s seniors. AARP is in fact a large, complex and sophisticated organization with over $2.2 billion in total assets and had revenues in excess of $1.4 billion in 2009 alone.
When measured by the products it endorses and profits it derives from those deals, AARP is one of the nation’s largest insurance companies and by far the largest provider of Medicare plans to seniors. AARP is also one of the most powerful and active lobbying groups (in terms of dollars spent) in the country.
Further clouding AARP’s image is a tangled relationship between the board members of its “for-profit” subsidiaries and the parent “non-profit” AARP which establishes AARP’s policy positions – often making it impossible to tell the two sides, and their competing agendas, apart.
Repeat Offender: Part 1, 2, 3 …
It should be noted that this report is not the first time AARP’s commercial activities have been the focus of federal government actions seeking to address a range of improprieties which appear to conflict with the organization’s 501(c)(4) tax-exempt status.
In 1994, AARP paid the Internal Revenue Service (IRS) a one-time settlement payment of $135 million in lieu of taxes, resolving an audit over tax returns for years 1985 through 1993 for failure to fully pay unrelated business income tax (UBIT) on its commercial activities.
Also in 1994, AARP agreed to pay the U.S. Postal Service $2.8 million to settle allegations that AARP improperly mailed health insurance solicitations at non-profit rates in 1991 and 1992. In 1999, the IRS and AARP once again reached a settlement to conclude an IRS audit of the organization covering tax years
1994 through 1998 with respect to the treatment of revenues AARP received from licensing and selling its name and logo to insurance companies. More than a decade later, AARP activities and business arrangements continue to raise concerns about which interests are being served at AARP – those of its 40 million members or the AARP business portfolio.
See full report: http://waysandmeans.house.gov/uploadedfiles/aarp_report_final_pdf_3_29_11.pdf
Tort Reform
To Sue or not to Sue… That is the question
 ”The first thing we do, let’s kill all the lawyers.” (Shakespeare in Henry VI, part 2, Act IV, Scene II). Shakespeare’s acknowledgment that the first thing any potential tyrant must do to eliminate freedom is to “kill all the lawyers” illustrates the central role lawyers have played in modern civilization, irrespective of weather that role is positive or negative.
”The first thing we do, let’s kill all the lawyers.” (Shakespeare in Henry VI, part 2, Act IV, Scene II). Shakespeare’s acknowledgment that the first thing any potential tyrant must do to eliminate freedom is to “kill all the lawyers” illustrates the central role lawyers have played in modern civilization, irrespective of weather that role is positive or negative.
The Positive
On the positive side, the legal profession has codified laws and drafted constitutions of many countries, giving recourse to the weak and oppressed against the powerful and privileged.
The Negative
On the negative side, the mercenary behavior of some lawyers has left the reputation of the field in tatters, with lawyers now occupying a status in society only a notch above bankers, stock market analysts and politicians (at least for the time being).
The Savings: If we changed…
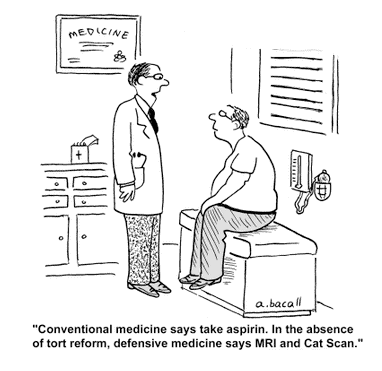
The Gallup Organization estimates $650 billion could be saved nationally from the health care system — more than one of every four dollars spent — if doctors, hospitals and other medical providers didn’t have to protect themselves from being taken to court by ordering unneeded tests.
The damage has been done…
Lawyers on the whole have done the most damage to the medical profession and ultimately to the supposed beneficiaries, the patients. The litigation threat has affected trust between physician and patient. Medical care should be driven by patient-physician respect, not by actions of lawyers. How can this rapport be established if the physician wonders about every patient being a walking lawsuit?
Dragging a physician to court for every perceived mistake, however small or understandable, has led to defensive medicine wherein all kinds of tests are ordered to avoid the remotest possibility of overlooking something. A physician should not have to conduct tests s/he does not think necessary but has to simply because it could be used against her or him in court.
A physician undertakes therapeutic interventions that s/he considers best for the patient. However, every medication or procedure has side effects or interactions that can be unforeseen and serious. A physician should explain the most likely and the rare but serious possible adverse outcomes. But it is impossible to list every single reaction for every single intervention and the physician cannot be held accountable.
Mistakes do happen…
It cannot be denied that medical mistakes are made, some egregious, for which the victim or patient should be compensated. However, there is no reason why that compensation should drive the average physician out of business by virtue of raising insurance premiums to ridiculous levels.
What can we do to fix the problem?
Tort reform has already been proposed to correct this anomalous situation, placing limits on payment for “pain and suffering”. However, to redress the balance, here are some other remedies that could be applied
- Lawyers should be liable for cases they lose by paying court cost and time spent by the defending physician. This should decrease frivolous lawsuits.
- Lawyers should not be paid a contingency of 30% – 50%, as is the case now. That amount should be reduced to not more than 10% of final settlement as has been proposed in Florida. Financial incentive should not be a driving force here, genuine concern for the litigant should.
- Lawyers who file more than a pre-specified number/percentage of frivolous lawsuits should be barred, just as doctors who commit medical fraud are de-licensed.
- Juries should be comprised of peers of physicians, nurses, and physical therapists, and physician’s assistants, under the supervision of judges. Juries should not comprise of those not intimately familiar with medical profession since they do not have the required knowledge to judge the appropriateness of medical care.
- Tort reform should also address a limit to malpractice claims, as is in Texas now.
Maybe when all the above changes are made, medical care will switch back to caring doctors and not sue-happy lawyers.
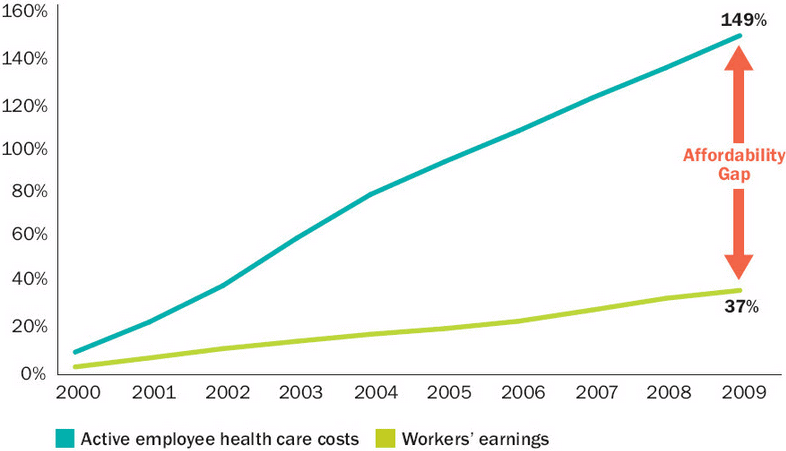
Healthcare Costs:
Medical related costs for almost every average American have grown so large that very few can actually afford coverage. Over the last decade we have seen costs of healthcare rise faster then our average wage, leaving many in the dark.
Here is a short excerpt that we found in Time Magazine about a man that was diagnosed with cancer that ran up a bill of nearly a million dollars before he died.
| By the time Steven D. died at his home in Northern California the following November, he had lived for an additional 11 months. And Alice had collected bills totaling $902,452. The family’s first bill — for $348,000 — which arrived when Steven got home from the Seton Medical Center in Daly City, Calif., was full of all the usual chargemaster profit grabs: $18 each for 88 diabetes-test strips that Amazon sells in boxes of 50 for $27.85; $24 each for 19 niacin pills that are sold in drugstores for about a nickel apiece. There were also four boxes of sterile gauze pads for $77 each.None of that was considered part of what was provided in return for Seton’s facility charge for the intensive-care unit for two days at $13,225 a day, 12 days in the critical unit at $7,315 a day and one day in a standard room (all of which totaled $120,116 over 15 days). There was also $20,886 for CT scans and $24,251 for lab work. |
Something isn’t right here
- It has been estimated that hospitals overcharge Americans by about 10 billion dollars every single year.
- One trained medical billing advocate says that over 90 percent of the medical bills that she has audited contain “gross overcharges”.
- Quote from Aetna’s CEO Bertolini, “In some markets, increases in premiums could “go as high as 100 percent. And we’ve done all that math. We’ve shared it with all the regulators. We’ve shared it with all the people in Washington that need to see it. And I think it’s a big concern.”
Conflict?
The chairman of Aetna, the third largest health insurance company in the United States, brought in a staggering $68.7 million during 2010. Ron Williams exercised stock options that were worth approximately $50.3 million and he raked in an additional $18.4 million in wages and other forms of compensation. The funny thing is that he left the company and didn’t even work the entire year.
So it is rather hard to listen to companies, when they say one thing about how healthcare will get more expensive but are in some ways contributing to the high costs by paying their C-levels absorbent salaries.
Medicare
It is America’s largest most likely to fail healthcare insurance programs. Medicare helps pay for healthcare for over 43 million people. But it is headed for disaster. Spending is growing faster then revenue due to America’s aging population.
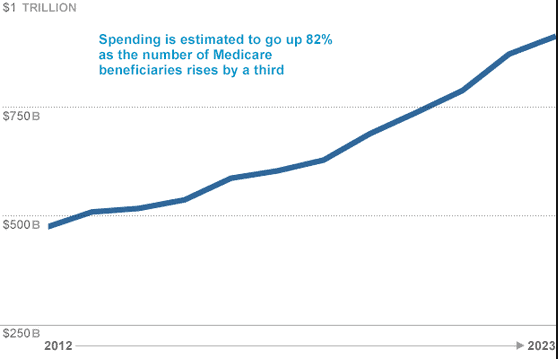
Medicare will not be able to pay for all the hospital bills that come in. Well before that year, Medicare beneficiaries will find that it is increasingly difficult to make appointments with specialists and gain access to high-tech care because of a squeeze on payments to providers. If trends continue, federal health spending (including the rising cost of Medicaid) will crowd out funding for the environment, defense, and other priorities from the budget.
How much does Medicare need to be saved?
Medicare will need about $10 trillion in new revenue (measured in today’s dollars) just to keep paying bills that will come in over the next 75 years for hospital care and other services under Part A. We will need about $20 trillion in tax revenue to pay for outpatient services under Part B and prescription drugs under Part D. Even in an economy as large as America’s (our GDP in 2006 was about $13 trillion), the tax increases required to raise such amounts would be formidable. Economic growth would suffer from the drain on the private sector and jobs would be lost. Although seniors might pay part of the needed costs, most of the burden of such a tax hike would be borne by our children and grandchildren.
Even if we raised the funds, much of the new money would be wasted without a fundamental reform of Medicare. Trying to maintain the program as it is today would mean preserving incentives for excessive and inappropriate care. While we need to ensure continued access to healthcare for Medicare beneficiaries, we should focus our efforts on creating a new Medicare program that works.
Thoughts on how to fix Medicare
- Change payment incentives. Medicare should pay for better health outcomes, not just for services performed.
- Enhance competition. As the Part D experience has shown, the best way to lower costs is through more competition, not more government management. Traditional Medicare should be permitted to adjust its benefits, premiums, and other features in response to changing consumer demand and evolving medical practice, rather than waiting for Congress to act.
- Improve care delivery. Traditional Medicare is “à la carte” medicine, with a vast menu of treatments and health providers laid out before often-uncomprehending patients. By failing to coordinate the delivery of health services, we waste resources.
- Keep track of which treatments work best. A flood of medical innovations promise improvements in our ability to diagnose and treat disease. Choosing a treatment can be complicated, however, and the knowledge of what really works is often lacking. Patient-level data from Medicare should be used to analyze the effectiveness of treatments for diseases.
- Let beneficiaries be consumers. When people turn 65, they do not suddenly lose their ability to make decisions. Fears that Medicare beneficiaries would not be able to select a Part D plan proved unjustified. To the contrary, that experience illustrates the need for a consumer-oriented infrastructure in healthcare. Consumers need transparency plus clear financial incentives that promote prudent decision making.
- Promote personal responsibility. Medicare should promote responsibility, such as better patient compliance with drug therapies for hypertension. The result will be better care and lower costs. But, again, the problem doesn’t begin with Medicare. Good health habits are developed well before age 65.
Doctors are going broke
 While most doctors (50%) are employed by hospitals, the other 50% may not be doing so good.
While most doctors (50%) are employed by hospitals, the other 50% may not be doing so good.
“A lot of independent practices are starting to see serious financial issues,” said Marc Lion, CEO of Lion & Company CPAs, LLC, which advises independent doctor practices about their finances.
Do more with less, much less.
Doctors list shrinking insurance reimbursements, changing regulations, rising business and drug costs among the factors preventing them from keeping their practices afloat. But some experts counter that doctors’ lack of business acumen is also to blame.
Loans to make payroll: Dr. William Pentz, 47, a cardiologist with a Philadelphia private practice, and his partners had to tap into their personal assets to make payroll for employees last year. “And we still barely made payroll last paycheck,” he said. “Many of us are also skimping on our own pay.”
Great with patients, terrible at business
I have seen this 100’s of times personally, doctors love their patients, want to help as much as possible but know very little about business (i.e. websites, Google Places, PR, marketing, software, etc…) It is shocking to see that most do not hire a quality business consultant to help assist with these types of duties. Most ask a staff, or family member to assist, and most are way under-qualified to help run an efficient practice.
Are you in this boat? not sure what to do with your marketing campaign?
Check out these articles we recently wrote, they should help.
- Developing a Great Marketing Plan – Affordable Best Practices (free e-book)
- 8 Quick Steps You Can Do Today to Set Your Healthcare Practice up for Gigantic Success
Meaningful Use
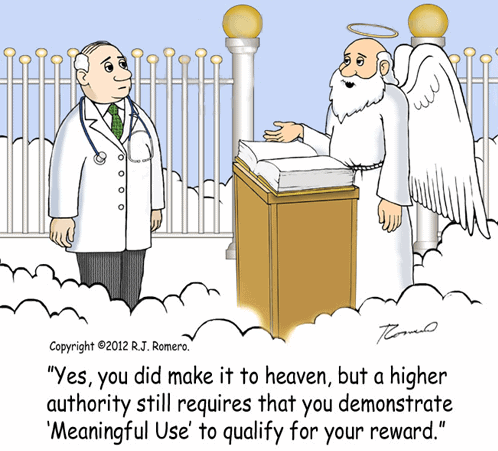 Unfortunately meaningful use and its incentives caused many problems that will be felt for years to come, it created a modern gold rush for new EMR vendors hoping to cash in. With that, very many vendors have created very poor systems that will probably fail in a few short years due to being designed incorrectly and not supported mainstream.
Unfortunately meaningful use and its incentives caused many problems that will be felt for years to come, it created a modern gold rush for new EMR vendors hoping to cash in. With that, very many vendors have created very poor systems that will probably fail in a few short years due to being designed incorrectly and not supported mainstream.
Stage 3 of the Medicare/Medicaid incentive programs for the meaningful use of electronic health records (EHRs) should not move forward until challenges associated with stages 1 and 2 have been studied and addressed, according to formal comments submitted to the Office of the National Coordinator for Health Information Technology (ONC) by the American Medical Association (AMA).
“The AMA shares the administration’s goal of widespread EHR adoption and use, but we again stress our continuing concern that the meaningful use program is moving forward without a comprehensive evaluation of previous stages to resolve existing problems,” said AMA Board Chairman Steven J. Stack, MD. “A full evaluation of past stages and more flexible program requirements will help physicians in different specialties and practice arrangements successfully adopt and use EHRs.”
The AMA outlined five issues it sees with the meaningful use program:
- No evaluation process exists. An external, independent evaluation is necessary to improve and inform the future of the program, the organization says.
- A pass rate of 100% is not “reasonable and achievable.” Failing to meet just one measure by 1% would make a physician ineligible for incentives and subject to financial penalties, according to the AMA.
- The program takes a one-size-fits-all approach, which is not appropriate. Program requirements should be more flexible and better structured to accommodate various practice patterns and specialties, the AMA says.
- The usability of certified EHRs is not addressed. The EHR certification process should address physician usability concerns, the group says.
- Health information technology (IT) infrastructure barriers need to be resolved. The health IT infrastructure does not enable physicians to readily electronically share patient data with other healthcare providers, according to the AMA, which says that infrastructure improvement to allow an efficient and secure electronic information exchange must be a priority.
With all these being said, we are in for one wild ride of regulation and failure and unfortunately both the doctors and patients will the guinea-pigs.
Over-Consumption by the Patient
Do you think, if patients were responsible for the dollars paid they may pay more attention to lifestyle, instructions from clinicians, consume less; would monitor what tests are being run on their behalf, would take more interest in their own care, own medical information, and maybe even choose more carefully what care providers they visited?
But alas, everyone is inherently lazy, they want an easy fix ; Fast food, fast answers, fast work-outs (if they do exercise at all).
Who makes the choice?
Does the patient, the doctor, the health insurance company, or the government decide when you do and don’t get care? When we talk about insurance companies, we talk about denying claims. When we talk about the government, it’s called “rationing”.
The simple fact is that someone rations care in every model:
- If consumers pay out-of-pocket, they ration care based on their willingness to pay. When a treatment is no longer worth the money, they “deny themselves” the care. Except in cases where the ability to pay comes into play, no one thinks twice about an individual denying themselves additional care. They may not even realize that it’s happening.
- If insurance companies bear the cost of care, consumers have no incentive to stop asking for more medicine and more procedures. This effect is known as the Tragedy of the Commons. Since the individual no longer denies themselves treatment but continues to bears the cost through higher premium prices, someone has to provide a financial control. Insurance companies, therefore, step in and deny coverage.
- Public health insurance is no different than the private sector. Consumers have no incentive to stop asking for more medicine or procedures and consumers bear the cost of this care through higher taxes so someone has to provide those financial controls.
Legacy IT Software Systems
 The current IT systems that providers have to maintain can be in the hundreds, some can even go as high as 1,000. Imagine having to manage 1,000 different software applications, and the vendors that are “supposed” to support them. It can be a nightmare.
The current IT systems that providers have to maintain can be in the hundreds, some can even go as high as 1,000. Imagine having to manage 1,000 different software applications, and the vendors that are “supposed” to support them. It can be a nightmare.
The current EMR/practice management solution operate more like a document management system, rather then a customer/patient customer relationship management application. The applications have no effective way to manage and track outreach to other providers which is critically needed.
So what can we do?
The good and the bad news. Most progressive healthcare providers are slowly updating their systems. The bad, when you have a 1,000 systems to update, the time-line equals decades, not years. So CTOs of major companies operate in band-aid mode always patching their current systems as they break in hopes that their systems don’t explode.
Problem:
Both the hospital staff that maintain the systems and vendors that build and maintain them are the problem. Many times non-technical people are assigned major decision making roles within the IT department. Why? Because no one knows any better and this causes many bad decisions to be made.
Check out this recent article about “6 Surprising Reasons Why Healthcare is NOT Ready for Innovation” which discusses why many hospital and clinics are in big trouble. You will be surprised with what you read.
Universal Coverage
 This is a touchy subject for most Americas. Those with healthcare argue that everyone should pay their own way, those that do not have coverage are asking “what about me?”. The problem arises that it is both a financial discussion and one of morality and compassion.
This is a touchy subject for most Americas. Those with healthcare argue that everyone should pay their own way, those that do not have coverage are asking “what about me?”. The problem arises that it is both a financial discussion and one of morality and compassion.
Should all Americans be guaranteed access to basic health and medical care? Should the child of an unskilled hourly worker have access to the same care options as the CEO of a large corporation, or a U.S. Congress member or a retired union member? Should there be differences in the care available from state to state?
Is healthcare a human right? like police or education? Or is it a social responsibility.
The problem goes a lot deeper, we know the financial implications for both the healthcare facility, the payer, and the patient. But what is not fully understood is how we make patients adhere to better system of prevention.
If you currently smoke, or drink, do you get the same benefits or pay the same as someone who does not? And who monitors these activities to make sure you pay your fair share. As we all know these are impossible to manage. Yet we are headed down this path.
America Stands Alone
According to the Institute of Medicine, one of the National Academies Sciences of the United States government, the United States is the only wealthy, industrialized nation that does not ensure all citizens access to healthcare as part of a universal healthcare system. By the end of 2009, 47 million Americans did not have health insurance, meaning, they could not access medical care without having to pay for it out of their pockets. The new law will make it possible for 32 million of them to get healthcare services by 2014, but do the math – there will still be 15 or 16 million who will still not have access to care.
The long, (really long) and the short of it
We as patients, doctors, vendors, or institutions have a very long road ahead of us, and it does not look like it will get any better fast. We all have to do our part, (mainly you) by working out, taking care of yourself, eating right so you can help minimize the effects of our environment and lessen the need of healthcare services.
Hopefully everyone realizes this is serious and if we do not change, we are in for big trouble in the years to come.
Wish you luck, and see you at the gym!