Compliance is a state of meeting the rules and regulations of any given program. When it comes to medical billing compliance, it is worthwhile to talk about it with America under the dark clouds of COVID-19, and healthcare dynamics continue to change as we speak.
On one side, we see Personal Protective Equipment (PPE) mandatory for both patients and providers alike; on the other, it is only possible to protect ourselves if we work together as a community. It is paradoxical. With that said, we explore the answer to the following question in this article:
How do practices adhere to the medical billing and coding rules during the pandemic?
Alongside this, we will look into the role of healthcare technology in critical times we currently experience. Healthcare IT is where innovation, experimentation, and execution of medical research happen. Unless we are technologically prepared to face challenges, we can’t ensure the delivery of quality care, patient safety, and a practitioner’s goal of clinical compliance.

Photo by Brian McGowan on Unsplash
AAPC brings Medical Billing Compliance Updates
American Academy of Professional Coders (AAPC) is the portal for medical billing and coding updates. It also carries the knowledge base to turn aspirants into medical billers and coders.
Practitioners, students, staff, and administrators should all use AAPC not to miss anything of grave importance. We derive some of the data from them to reach authenticity and transparency in our content.
The generic term under which medical billing compliance falls is healthcare compliance. Practitioners must follow these rules to avoid coming under the government’s scrutiny. Whether it is a COVID-19 health emergency or not, practices are under obligation to observe medical coding regulations; follow federal and state laws for claim submission; translate provisions of the HIPAA law into action, and understand Occupational Safety and Health Administration rulebook.
Healthcare Technology is at the Heart of It
United States Office of the Inspector General (OIG) governs medical billing standards, and they do not change while COVID-19 continues to spread. The good news for clinicians is the announcement of COVID-19 diagnostic and treatment codes using a COVID game changer for physicians.
Medical billing services such as ours continue to track compliance standards and return with maximum reimbursements for rendered services. Practices suffer from a surge in patients as America reopens and life gets back to the new normal. The world now is changed compared to the world we used to live in! We see a lot of empathy for survivors and prayers for those who are not with us anymore.
Our healthcare heroes deserve all the credit for creating the world’s best care system. Even though we see overwhelming deaths, if we manage to save one person from COVID, the whole country wins.
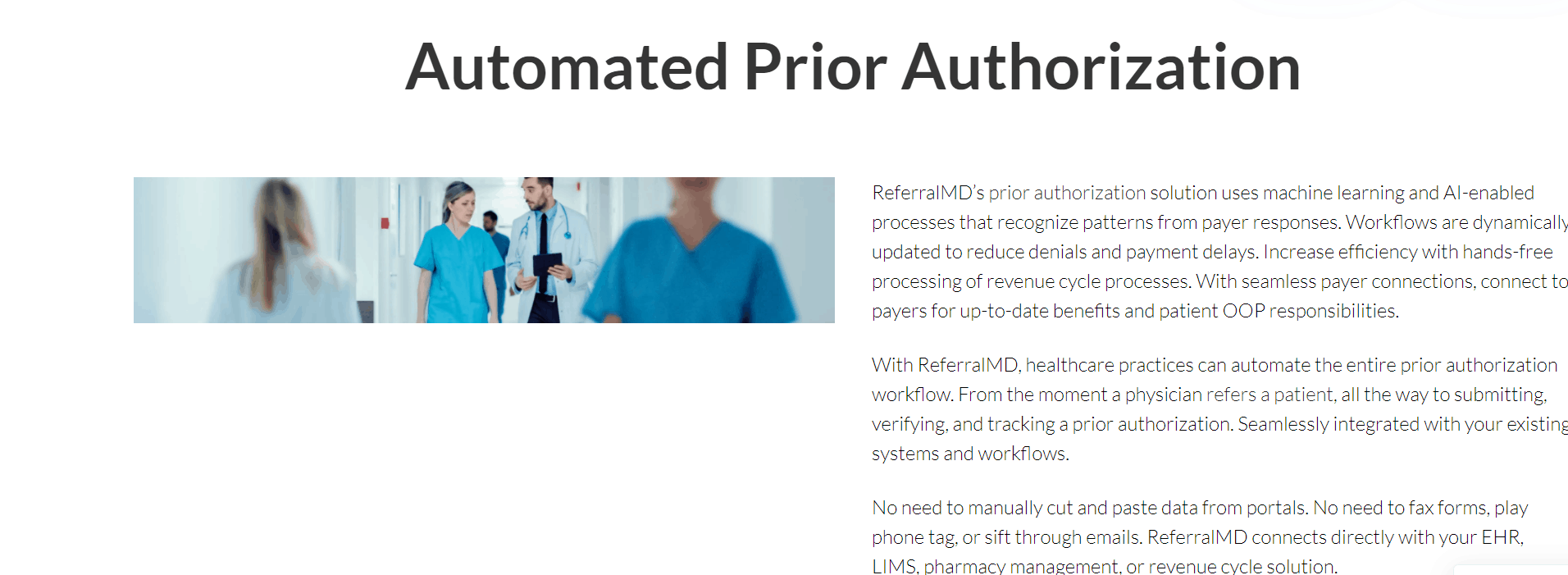
Prior Authorization: Medical Billing Essentials
Billing claims are one of the standard transactions to be completed electronically under HIPAA. Manual billing has certain drawbacks. In comparison, electronic submissions mean fewer errors, high acceptance rates, and faster collections.
The process of prior authorization, also known as preauthorization, means to set up a contract with the payer to pay for specific services before a provider conducts them. It is an essential component of modern medical billing services. The medical billing companies rely on it as part of their revenue cycle management process for providers.
Before the insurance companies authorize a service, they release an authorization code to be included on the claim for approval. The trick here is to add the right CPT code of the service, a task usually mishandled in routine. Therefore, coders need to be super careful about it.
Healthcare management duties involve proper coordination with physicians on what they anticipate doing. As a business partner of practices, one must predict all possible situations; otherwise, you are at the hands of a falsely coded claim, and denial of payment becomes inevitable.
In the current air of uncertainty, the anticipation of COVID-19 related procedures and application of relevant codes is where the skills of medical coding teams matter most.
Telehealth via Zoom Prioritizes Patient Safety
At first, the Zoom app is HIPAA compliant and comes under the allowed set of apps by CMS. PHI or protected health information that includes patient data and other sensitive information has to remain private at all times. And, Zoom offers that exactly. HIPAA law protects such information when it goes public through penalties, fines, and even jail time in some cases.
The medical billing process involves transmitting sensitive data through computer systems built with safety, integrity, and storage protocols in place.
To minimize exposure to COVID-19 germs, patients take the route of video consults with physicians. Zoom, in particular, stands out as the most used app, especially when it comes to physical therapy over the past few months, says APTA’s June 2020 survey.
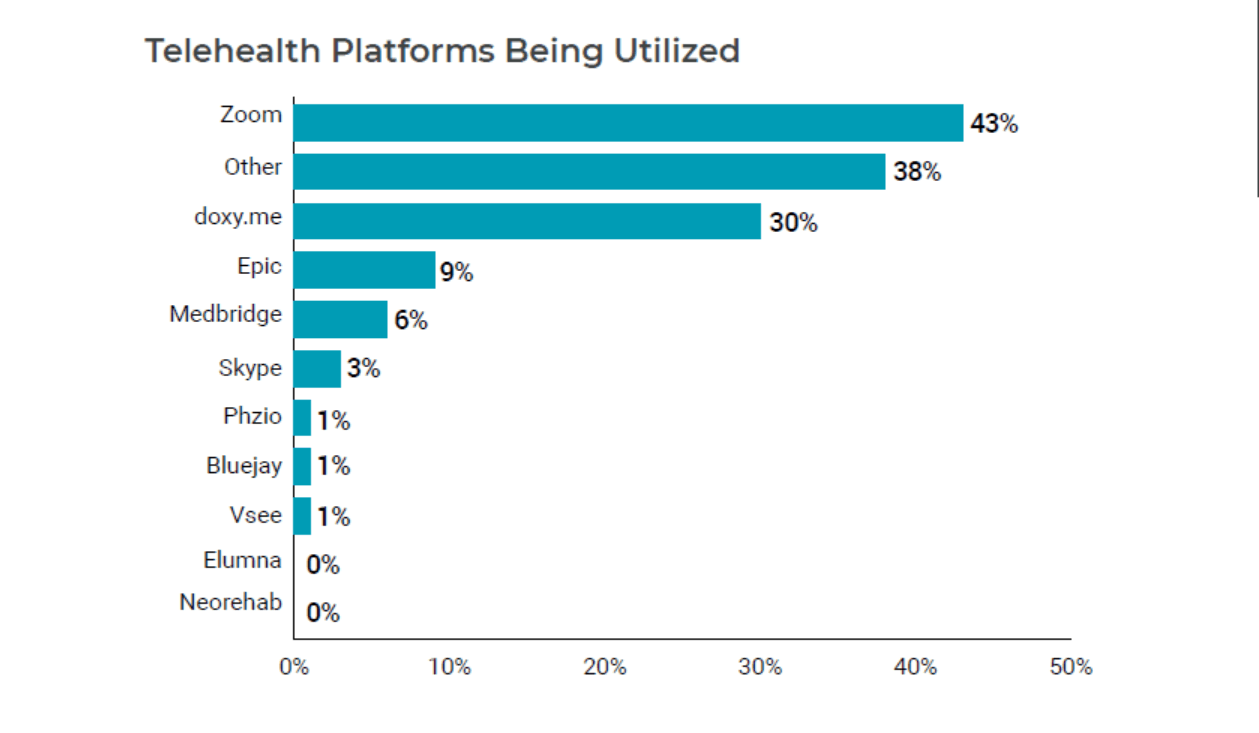
While hospitals, clinics, and private practices open up and carry on with the delayed procedures, telehealth continues to reimburse practitioners.
The growth of your medical practice in 7 easy steps is a quick guide to scaling your medical practice. It takes you into the world of workflow smoothness by measuring clinical progress, increasing patient volume, and maintaining safety standards.
Be Wary of Statutory Health Laws
By keeping an eye on CMS updates concerning Medicare and Medicaid insurance programs, clinicians can meet medical billing compliance in the new normal. Under the current scenario, they have gained increased importance. With corporate companies closing down stores, we can be sure of the government enforcing the law to affect. Such implementation requires us to stay on our toes and be vigilant at all times.
Talking about the law, the Department of Health and Human Services (HHS) made a special announcement for providers recently. They asked providers to ensure the payment for their services regarding COVID-19 testing and treatment of uninsured patients.
Henceforth, to be fully in charge of your revenue cycle, it is vital to stay informed. Moreover, for proper reimbursements, claims with the right codes and correct charges resolute success; last but not least, a medical billing company with experience paves the way for constant recovery.









