As social distancing remains our chief tool to fight COVID-19, telemedicine is becoming the go-to strategy to help every medical facility keep its staff and patients safe. Here’s how telemedicine can help your practice during COVID-19 and remain a constant in your practice following a return to normalcy.
The onset of the COVID-19 pandemic will be remembered for many things beyond the illness itself. From our unprecedented international response to a devastating illness to the broader socio-economic implications of social distancing, this time in history will be lauded, discussed, and even condemned as each organization and individual responds to the crisis. As social distancing remains our chief tool to fight COVID-19, telemedicine is becoming the go-to strategy to help every medical facility keep its staff and patients safe. Here’s how telemedicine can help your practice during COVID-19 and remain a constant in your practice following a return to normalcy.
Heroes have emerged from the pandemic. Our frontline healthcare workers and the institutions that support them have amassed an unprecedented response in the fight to save lives. Still, companies have also fought hard to shift manufacturing processes to wartime mask and ventilator production. Governments have played a part in crisis communications that have saved lives. But a quieter hero is also at the forefront of this fight that is as close to you as the smartphone you’re using to read this article.
So, let’s talk about how telemedicine can help your practice now and what it means for patients following the coronavirus outbreak.

Photo by National Cancer Institute on Unsplash
What is Telemedicine?
Telemedicine, telehealth, e-health (electronic health), and m-health (mobile health) are commonly associated with telecommunications technology that allows clinicians to provide remote medical treatment to patients. The technology has been in use for decades but has yet to see widespread adoption—until now. More than 10,000 peer-reviewed publications in the past 20-years have studied the application of telemedicine as a viable alternative to the traditional in-office visit.
The phrase “telehealth” designates a category of healthcare technologies that allow clinicians to treat remote patients from their practice setting. Telehealth encompasses the entire service line of applications that can include clinical and non-clinical services. Non-clinical telehealth applications could include virtual provider training, video conferencing meetings, or other continuing educational pursuits.
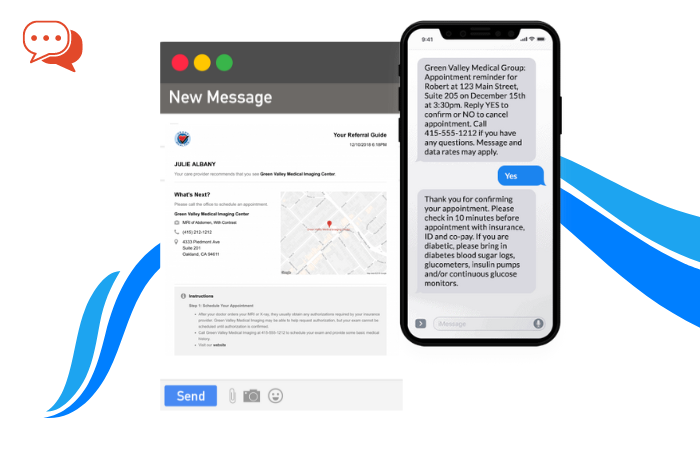
Telehealth tools leverage digital telecommunications technologies, including your wireless connectivity to the Internet, application software for video conferencing, texting, or relaying data with the use of common digital devices such as your smartphone, laptop, tablet, or desktop.
Telehealth services are divided into separate technology categories:
- Asynchronous telehealth, or store-and-forward technology, transmits recorded medical data to a practitioner for later viewing. This commonly includes case histories, images, audio recordings, or other information. Often, asynchronous telehealth leverages the second opinion of a specialist.
- Synchronous telehealth is two-way communication between a clinician and patient separated by distance. This is typically handled through a telemedicine software application with a videoconferencing feature. It’s a way to provide face-to-face interaction with a remote patient for education, diagnosis, and treatment.
- Remote patient monitoring uses technology tools to track patient symptoms from a remote location (usually their home) and then transmit them to a hospital or other clinical facility.
The term “telemedicine” applies to the clinical application of telehealth technology. Today you will find telemedicine hard at work in a variety of settings; Care providers use telehealth technology for:
Digital remote monitoring for chronically ill patients at home or another remote setting.
- Doctor-to-doctor consults for better patient care coordination.
- Mental health counseling encounters.
- For sick inmates in locked down federal correctional facilities.
- Bedside clinical on-call doctor visits for nursing homes.
- Patient education around medication management.
- On-call specialty consultations for rural hospital ERs.
- Immediate on-site triage of workers’ compensation.
Telemedicine can be used for a variety of chronic or non-urgent consults. Whether the visit is a routine post-surgical checkup or a non-urgent consult by a primary care doctor, these tools bring medical treatment to patients no matter where they are located.
While these are a few of the telehealth applications commonly used today, telemedicine has risen to the forefront of patient care during the COVID-19 pandemic.
How is Telemedicine Being Used During COVID-19?
Roughly 80% of American hospitals leveraged telemedicine by 2017. Despite this, patients, and many doctors, have been slow to use these tools. Doctors expressed reluctance to shift the traditional patient encounter to one dependent upon technology. This, despite the accumulation of decades of data showing the quality of care during a telemedicine visit, is just as high as a traditional office visit.
Reimbursement barriers to telehealth have also remained a consistent problem. As a result, few medical practice providers and even many hospitals refused to market the service or even adopt these tools and accompany clinical and operational workflow changes. But patients show less reluctance; surveys show that the American public seems to be primed to try out the convenience of telehealth.
With the onset of COVID-19, telehealth technology usage skyrocketed practically overnight. Telemedicine had long been seen to provide care during the outbreak of flu epidemics in the past. But with a virus 20 to 30 times more deadly than the flu, no vaccine, and a shortage of critical medical supplies, telehealth quickly became the recommended way to provide care.
Telehealth tools can help healthcare providers fight COVID-19 by:
- Keeping Social Distancing
Smartphones or tablets can facilitate communication between at-risk patients with chronic diseases and their care providers, keeping them at home and away from populated settings like an ER or practice waiting room. Home monitoring can take the place of a routine checkup for patients with diabetes or chronic heart failure. Telemedicine is also a proven technology to provide mental health counseling and patient education. - Triaging Flu Patients
The “worried well” has overwhelmed hospitals. Telehealth can give these patients an alternative to an ER visit where, if they weren’t already a carrier, they face exposure to the coronavirus. Patients experiencing moderate flu symptoms can be treated at home to lessen the pressure felt by overtaxed ERs. This prevents the spread of COVID-19 by keeping people home. - Protecting Healthcare Workers
In addition to lessening the work of harried ER teams, telemedicine can keep distance between non-urgent but communicable patients with minor COVID-19 symptoms and healthcare providers. A virtual visit can limit healthcare worker exposure, particularly in medical practices that continue to see patients during this time.
With telemedicine, providers can effectively evaluate potentially infected patients. If the patient is presumed to have mild symptoms of the virus, they will likely be asked to stay home and monitor the disease progression since few test kits and no vaccinations are available. A virtual consult can help monitor these patients and provide care to keep them comfortable or advise them on when to seek an ER visit, with no risk of exposure to the clinician or anyone else they encounter.
Organizations recommending telehealth technology in the fight against COVID-19 include the Centers for Disease Control (CDC), the American Hospital Association (AHA), and the Centers for Medicare & Medicaid Services (CMS).
In April 2020, as part of the federal government’s stimulus relief package, CMS announced a series of sweeping changes to telehealth reimbursement. In addition to enforcing payment parity for a telehealth visit at the same rate as an in-person encounter, CMS also dismantled many of the barriers to telehealth reimbursement that have kept many providers from adopting these tools. Under the new decision, Medicare patients can receive telehealth services at home, and doctors can be reimbursed just like for an in-person visit.
Since most hospitals and their ambulatory providers already have telehealth technology in place, shifting patients to a virtual consult, while not easy, is certainly possible. But rural community providers and smaller or independent medical practices may find the cost of implementing sophisticated virtual patient portals prohibitive. Traditionally, commercial video conferencing solutions such as Facetime were not HIPAA-compliant. But in early March 2020, the HHS Office for Civil rights said it “will use discretion” when enforcing HIPAA-compliance for these tools. HealthcareITNews reported the ruling says clinicians can use any audio or video communication technology to reach patients where they live to provide care, “regardless of whether the telehealth service is related to the diagnosis and treatment of health conditions related to COVID-19.”
Circumstances have aligned in a way that makes telehealth technology feasible for any medical provider and necessary to preserve and promote public health.
If your medical practice or a smaller healthcare facility is ready to try telehealth, there are some best practices to share before getting started with telemedicine.
How Can a Smaller Healthcare Practice Get Started With Telemedicine?
The first step toward launching a telehealth service line in your practice or small hospital is to select the technology provider. We recommend searching for a HIPAA-compliant software application simply because the current rules relaxing privacy concerns are temporary. Once your telemedicine practice is established, you will not want to switch providers should the rules change post-pandemic. Look for software that builds patient consent directly into the upfront processes and encrypts protected health information.
The platform you select should be a plug-and-play SaaS (software-as-a-service) offering that is subscription-based. This will lessen both your upfront and monthly recurring costs. These carriers can be implemented with a simple download and do not require any additional equipment beyond an Internet connection, Wi-Fi, and hardware with a camera, whether smartphone, tablet, laptop, or desktop.
Look for customizable software, so your practice can brand the tool with your name and choose workflows such as a method for patient registration, a virtual queue or waiting room, a way to archive the encounter, and interoperability with your electronic medical records (EMR) platform. Ideally, you would want to embed the telemedicine link directly on your website. One-click could start the registration process.
Security is an important consideration for any technology. The best software encrypts data, has no publicly sharable links, and allows for personal verification during the virtual visit.
Small providers should also carefully consider telemedicine’s impact on existing workflows and staff responsibilities. It’s a good idea to reach out to your private payers to determine proper telehealth billing procedures. Click here to read more about telehealth CMS reimbursement.
But the physical space of your practice may need to shift. A telemedicine visit requires a quiet professional space within your practice, whether it’s a designated exam room or practice manager’s office where these visits are conducted. Pay attention to the view behind the practitioner; a bookshelf or a blank wall over a crowded supply closet provides a more appropriate setting. Select a location with a door that closes or, at a minimum, lacks back and forth traffic flow to comply with HIPAA privacy rules.
As an alternative, telehealth could launch as an after-hours service from the comfort of the provider’s home. However, the same rules for the physical space and telehealth practice etiquette still apply.
It’s a good idea to set up a telemedicine superuser who can serve as the liaison between the telehealth technology provider and the practitioners. Your telehealth vendor is often a good source for advice and support that extends beyond the software they offer. Some of these technology partners work with marketing firms to help you roll out your telemedicine service line.
Finally, it’s time to roll these new workflows out to your patients. Today, one logical area to rollout telemedicine in your small practice could be simply as a triage for COVID-19 patients. If this is your focus, practice messaging could direct patients to a one-click button on your website or a downloadable app that schedules the patient encounter. On-hold practice messaging should reflect the telemedicine alternative along with signage on your doors and in waiting rooms. Receptionists should be well-aware of these triage protocols and work to funnel potential COVID-19 patients into the telehealth queue.
Telehealth During Coronavirus
Ultimately the efficacy of telehealth to drop the COVID-19 infection curve is yet to be documented. But the virtual video visit has been proven effective so far in mitigating the risk to both patients and providers.