The prior Authorization process has been a hot topic of debate in the healthcare industry for some time. Yet as with any healthcare process and procedure, there are pros and cons to the payment authorization process.
What is prior authorization in healthcare?
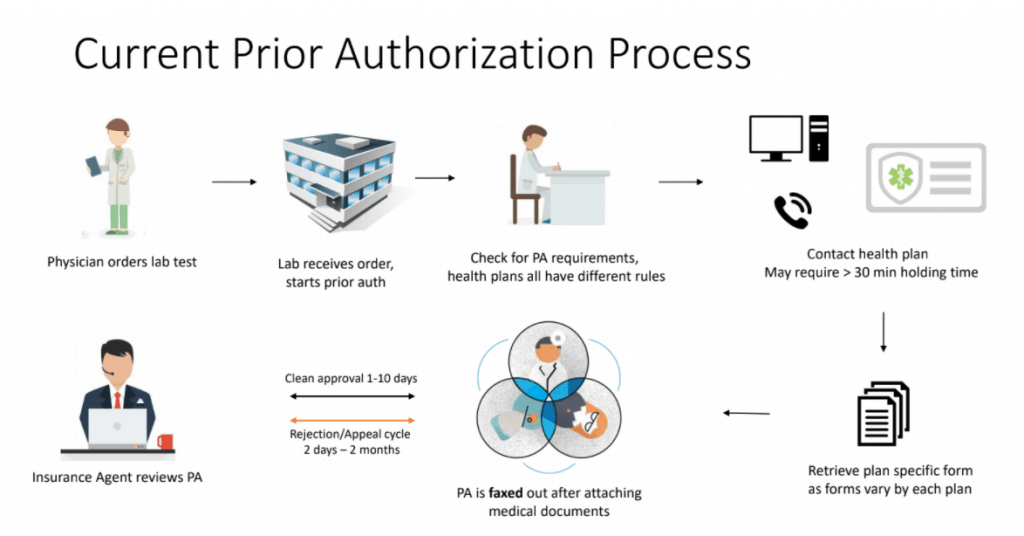
Prior authorization (PA or prior auth) is often used with expensive prescription drugs. Health insurance companies use prior authorization to verify that a certain drug, procedure, or treatment is medically necessary before it is done or prescribed. Put simply; it is the process of getting approval from your health insurance company (not your doctor) to obtain a prescription or treatment as demonstrated below:
Although a lengthy process, the ultimate purpose of PA is to optimize patient outcomes by ensuring that they receive the most appropriate medication while reducing waste, error, and unnecessary prescription drug use and cost, it is about keeping healthcare costs in check. With health insurance companies having more control over which prescriptions they will pay for; they can provide more expensive medications to those who truly need them.
The chart below illustrates the two types of processes for prior authorization of a prescription, “soft” and “hard” PA.
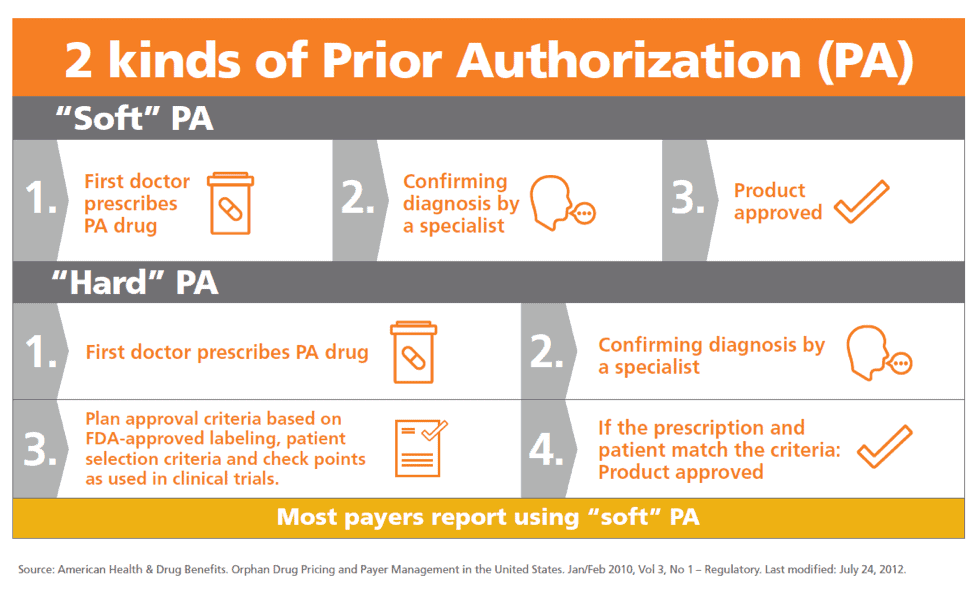
Hard and Soft Prior Authorization Process
Image source: Optum
Most payers often follow “soft PA”. First, your doctor will prescribe the prescription to you. If a prescription requires authorization, the pharmacy will contact whoever prescribed the medication (physician) and will let the physicians know the insurance company requires a PA. At this stage, the patient can choose to pay for the prescription themselves or wait for authorization from the insurers. Next, the physician will contact the insurance company, they will have to fill out forms and submit a formal authorization request to be reviewed. Ultimately, the product is approved.
Hard PA is where physicians have to submit more information due to a failed authorization. This can result in a requested service being denied, or an insurance company requiring the patient to go through a separate process. This process can take up to a few days to be completed, and if the prescription matches the criteria, then the product or treatment is approved.
To learn more about Prior Authorization with ReferralMD
Can prescriptions get rejected?
Around 66% of prescriptions that get rejected at the pharmacy require prior authorization. When a PA requirement is imposed, only 29% of patients end up with the originally prescribed product—and 40% end up abandoning therapy altogether! Not only is this negative for pharmaceutical organizations, but most importantly this causes frustration to patients who don’t get the medication that could best treat their condition, or who don’t get any therapy at all. (ReferralMD has a solution for Prior Auth which speeds the process and reduces denials)
What kinds of medications require prior authorization?
There are many reasons why a medication may require prior authorization. The criteria where a prescription may need authorization is if:
- The brand name of a medication is available as a generic. For example, Drug A (cheaper) and Drug B (expensive) are both able to treat your condition. If the doctor prescribes Drug B, your health plan may want to know why Drug A won’t work just as well.
- An expensive drug (as with psoriasis and rheumatoid arthritis medications)
- Medication used for cosmetic reasons (such as hair growth)
- Higher doses of medication than normal
- Medication that treats non-life-threatening conditions
- Medication is not usually covered by the insurance company but is deemed medically necessary by the physician (who must also inform the insurance company that no other covered medications will be effective)
- Drugs that are intended for certain age groups or conditions only
- Drugs that have dangerous side effects
There is a list of reasons why PA is required. Although prior authorization is designed to control costs, in practice this requires a lot of administrative time, phone calls, and recurring paperwork by both pharmacies and doctors as shown by the steps involved. Below, we go through the problems the process presents and why it is so hard to manage.
- Consumption of Doctor’s Time
Many physicians have long expressed their dissatisfaction with the time they and their staff have to spend interacting with health plans according to Medical Economics. When a prescription needs authorizing, this takes a lot of admin time, including the time a physician has to spend persuading an insurance company to cover a medication or a procedure that is expensive.
For most prior authorizations, physicians have to follow multiple steps. This can involve securing the correct form, filling the form out with the required information, submitting the form to the plan, etc. In particular, the holding time is long when trying to reach a customer service representative in the insurance company, with hold times averaging 20 minutes or more. Many physicians will tell you that the overall process can take 30-45 minutes for each PA submission.
There are many real-life case studies that demonstrate the inefficiencies of PA. Danielle Ofri, an associate professor at New York University School of Medicine, speaks of her experience with PA as “frustrating.” In one example, Dr. Opri had to go through four phone calls and four customer-care representatives to get the request of 90 pills each month for her patient who suffers from high blood pressure, rather than the 45 which was recommended by the company. The issue was that 45 pills a month was the maximum allowed for this particular medication. After submitting a list of information including a list of all the blood-pressure medications that the patient had been on in the past, including dates of initiation and relevant lab values, Dr. Ofri was able to get approval from the representative after going back and forth countless times. According to Dr. Ofri, the time spent on the phone could have been put to better use for patient care.
 Kevin de Regnier, DO, a solo family practitioner in Winterset, Iowa, also speaks of his negative experience with prior authorization which has grown steadily during his 26 years of practice. According to de Regnier, nurses spend about 10% of their time each day on prior authorization. “It’s an unreimbursed cost of providing care, and unfortunately we don’t have the financial resources to bring in someone to do prior auth exclusively, even on a part-time basis,” he says.
Kevin de Regnier, DO, a solo family practitioner in Winterset, Iowa, also speaks of his negative experience with prior authorization which has grown steadily during his 26 years of practice. According to de Regnier, nurses spend about 10% of their time each day on prior authorization. “It’s an unreimbursed cost of providing care, and unfortunately we don’t have the financial resources to bring in someone to do prior auth exclusively, even on a part-time basis,” he says.
Unfortunately, they are not alone; a survey found that 84% of responding physicians believe the burden of PAs is high or extremely high. Another 86% of physicians also responded that the burden of PAs has increased over the past five years which takes away the time that physicians can care for their patients.
2. The real cost of PA
Although PA has been an issue among healthcare providers for many years, little is known about the cost, either to individual practices or the healthcare system as a whole. In 2009, one study estimated that on average, prior authorization requests consumed about 20 hours a week per medical practice: one hour of the doctor’s time, nearly six hours of clerical time, plus 13 hours of nurses’ time.
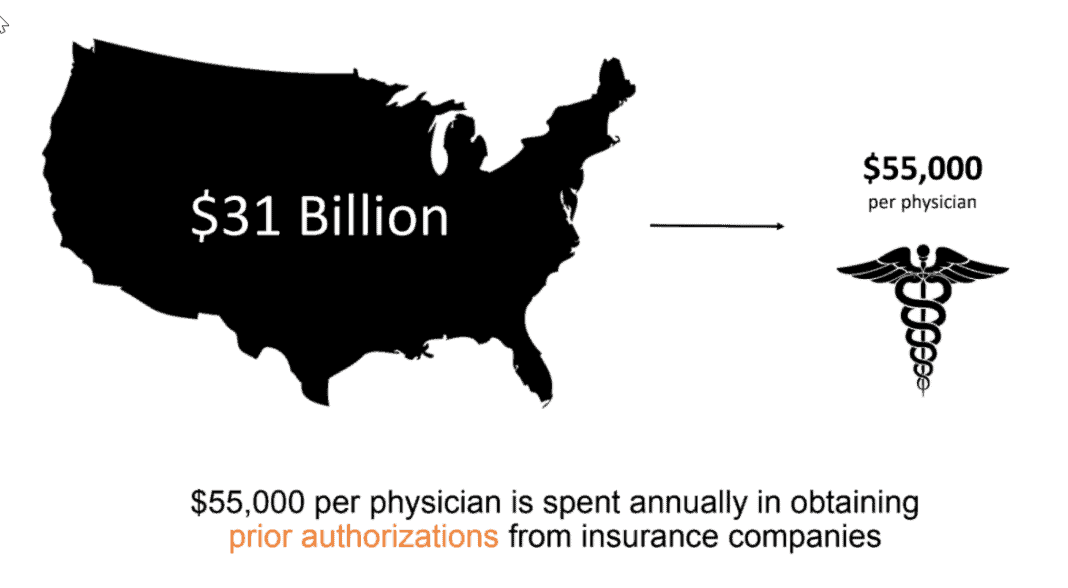
A study by Health Affairs further revealed that when the time is converted to dollars, practices spent an average of $68,274 per physician per year interacting with health plans. This equates to $23 billion and $31 billion annually! Prior authorization ultimately ends up costing the healthcare system more than it saves.
3. Prior authorization predicament
More drugs than ever before require PA, and the number of insurance plans is growing too—each with its own forms and policies. This makes it difficult for providers to keep up as they often change with regularity.
Failure to obtain proper authorizations can have a drastic effect on the practice income. No authorization means no payment. Insurers won’t pay for procedures if the correct prior authorization isn’t received, and most contracts restrict you from billing the patient. PA denials result in lost revenue, declines in provider and patient satisfaction, and delays in patient care.
The chart below demonstrates this and shows how much revenue is lost due to authorization.
Despite the effort to save costs on the insurer’s side, it is not even clear whether insurance companies are saving money in the long run. One study examined the records of more than 4,000 patients with Type 2 diabetes who were prescribed medications requiring prior authorizations. Those who were denied the medications had higher overall medical costs during the following year; not getting the medications probably worsened their conditions. Therefore it cost insurers more in the long term as they seek other treatments and medication.
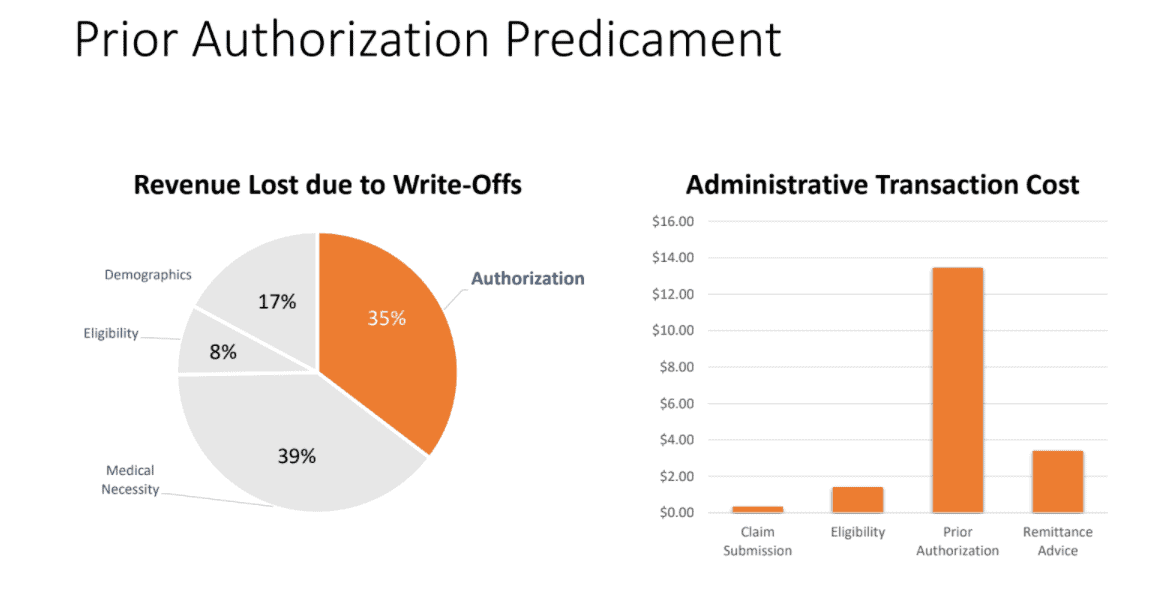
Although PA is widely implemented as a cost-containment measure, it is a labor-intensive procedure for health care providers, patients, pharmacists, and pharmacy benefit plans. Denied claims create the need for manual intervention; this increases practice costs and administrative transaction costs (just under $14 per transaction).
A common problem with many busy practices is that many claim denials sit unworked since denials are usually the most difficult and time-consuming work for billing staff. PA requires multiple letters with supporting documentation and multiple telephone conversations. As a consequence, PA costs are expensive, administratively daunting, and unsustainable for most primary care providers.
4. Patient delay
The real impact of PA is often felt by patients who are delayed in getting their medication or treatment. As a patient, PA problems can create a huge interruption; they have to figure out whether the process is stalled out by the doctor, the insurance company, or the pharmacy.
Nearly all physicians noted that wait times corresponded with delays in necessary care, which added to the risk of adverse events. Significantly, 78% of respondents said that PAs could result in patients forgoing necessary treatments, according to the release.
Up to 92% of doctors say that prior authorization harms patient access to care, which ultimately damages clinical quality outcomes. While the process brings a certain accountability and cost containment; several hours are lost in productivity.
For a submission to get authorized, approximately 64% of physicians waited for at least one business day for a PA decision, and 30% said they waited 3 or more business days, according to the AMA. During this time, patients are unable to start treatment. These long wait times have a negative impact on patient experience and patient care, and for many practices, the burden of the PA process causes them to abandon a preferred therapy in favor of a different formulary medication.
5. Management of PA
The management of PA can sometimes be difficult to manage as the requirements can vary widely from one insurer to another, each of which also has a different process for submitting prior authorization requests. This means the process cannot be standardized at times and must be done manually, which of course can drain resources and time if this is already limited.
Even when the practice has provided a request in a timely way, the insurer may still end up not paying for the prescribed medication or treatment. Unfortunately, claims with prior authorizations are denied more often than you might think. Insurance companies can deny a request for prior authorization for reasons such as:
- The doctor or pharmacist didn’t complete the steps necessary
- Filling in the wrong paperwork or missing information such as service code or date of birth
- The physician’s office neglected to contact the insurance company due to a lack of time
- The pharmacy didn’t bill the insurance company properly
- Outdated information – claims can be denied due to outdated insurance information, such as sending the claim to the wrong insurance company
- The insurer failed to notify the pharmacy
- The approval expired after a limited time (normally 30 days)
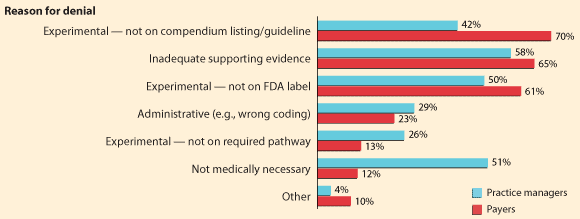
The chart below shows the reason PA was denied:
Graph of Prior Authorization Denial Reasons
Image source: Managed Care
From the chart, it is clear that the majority of payers report their denials due to the failure of physicians not meeting their guidelines – 70% of payers say that they deny requests because what is sent over is not consistent with their listing/guidelines. Whereas from the practice manager’s perspective, 42% of requests were denied due to them not meeting the guideline, therefore there is a slight discrepancy between the two.
One significant difference in perception between the practices and payers, however, is the denials for medical necessity. Only 12% of payers say they base their denials on medical necessity, yet 51% of practices say they receive denials for this reason. Payers and physician practice managers have different perceptions of why authorizations are denied.
What can be done to improve the Prior Authorization process?
- Electronic systems
Although PA is an unavoidable step in many practices. The current process is all too often manual and involves prescribers, payers, pharmacists, and patients in a cumbersome flow of information that may result in delays in treatment and dissatisfaction for all. As a result, many are implementing electronic prior authorization solutions to address common issues with the approvals process. Electronic Prior Authorization integrates directly with electronic health records (EHRs), enabling healthcare professionals to easily obtain prior authorizations in real-time at the point of care. This also eliminates time-consuming paper forms, faxes, and phone calls.
In 81% of instances where claims are denied, prior authorization was either not obtained or not handled properly. Electronic Referral Management Software can initiate automated prior authorization processes for hospitals, which in turn helps reduce front-end denials. Healthcare further revealed that prior electronic authorization could save as much as 416 hours per year! In 2015, the average cost to a provider for a fully electronic prior authorization was $1.89 compared to $7.50 for entirely manual authorization.
Interested in automating your prior authorizations? ReferralMD can offer a solution for referral workflow, e-consults, decision support, patient-provider matching directory, and prior authorizations; all within your current EMR system.
- Be familiar with the insurer’s policy
To reduce patient delay, it is vital that physicians check prior authorization requirements before providing services or sending prescriptions to the pharmacy. The two most common procedures that insurers require pre-authorization for are imaging procedures such as computerized tomography (CT) scans and magnetic resonance imaging (MRI), and brand-name pharmaceuticals.
Subsequently, Doctors should be familiar with insurers’ requirements and develop a list of drugs they all cover for common diseases. For example, if there are multiple choices for medications to treat diabetes, and you know the insurer will cover a generic drug, then get in the habit of prescribing that drug, providing that this is appropriate for the patient. This way Doctors can avoid the issue of dealing with PA and patients can gain quick access to their prescriptions.
- Employ a centralized system
Practices can often create greater efficiencies by centralizing the prior authorization responsibility. Many practices and health systems currently lack clearly defined roles when dealing with PA or simply do not have enough time. Putting just one or two individuals or a department in charge of prior authorizations for the whole practice will enable those employees to become highly skilled in the process and develop relationships with the payers. A centralized system also addresses the lack of consistency and ensures a more reliable and stable approach.