Healthcare and healthcare reform are topics for endless debate in this country, and have been since Teddy Roosevelt was president and ran for reelection on a platform that included national health insurance. The Affordable Care Act (ACA) is the latest incarnation of Roosevelt’s ideas, and just like in 1912 the subject has its supporters and its detractors. What most people agree on is that healthcare should be available to everyone rich or poor; no matter race, gender, or religion; or whether they live in the city or the country. But in the United States today, people who live in rural America are falling through the cracks.
Approximately 20% of the US population lives in rural America. Hospitals in non-urban areas are suffering; 43 rural hospitals have closed since 2010, 24 of those in the last two years, which is double the pace of the previous two. There are a number of reasons for these failures:
- Many states chose not to expand Medicaid and have suffered cuts in reimbursement.
- Most rural hospitals run on smaller budgets and cannot afford to meet the demands of the ACA that healthcare providers use electronic health records (EHRs).
- Most hospitals, large or small, are registered as non-profits, which means they must provide a certain amount of community benefits to receive tax exemptions.
- Fewer physicians want to work in rural areas.
The rural hospital is endangered and that means rural communities face health crises for all their citizens. Heart attacks, strokes, and traumatic injuries all require immediate intervention and an hour or 90-minute drive to an urban hospital can mean a death sentence. This is where the advent of telehealth could prove life-saving.
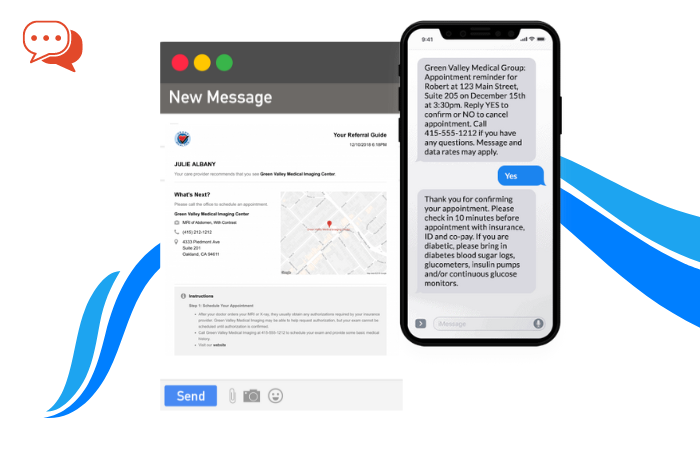
Telehealth is a growth industry that uses all the amazing communications inventions available today (wireless equipment, two-way video, smart phones, email, etc.) to connect patients and providers across the country. Telemedicine is not a medical specialty but a system by which hospitals and even private physicians can stay in touch with their client base. Services that can be provided include:
- Primary care and specialist referral services
- Remote patient monitoring
- Consumer medical and health information
- Medical education
Telemedicine can provide many means for resuscitating a community’s hospital and thereby a community’s health. The benefits are not just in physical health, but also in the emotional, educational and economic health of the area.
- Improved access to specialists – Geographic location is no reason these days for patients not to see the doctor—literally. Remote access services including teleconferencing, video-streaming and tele-presence robots, tablet and smart phone apps, can all be used for face-to-face interaction between patients and healthcare providers including physicians, nurses and physical therapists. Wearable and portable monitoring systems mean that healthcare providers can read real-time data from simple vital signs to more complicated heart rhythms without actually being in the same room as the patient.
- Improved clinical outcomes – Patients are diagnosed and treated earlier. Advanced ehealth care techniques are available at the touch of a button. Stroke, trauma, and intensive care services and monitoring can be provided immediately, within minutes of an event instead of within hours of travel time. All of this lessens complications, days spent hospitalized and mortality rates.
- Increased patient satisfaction – The emotional benefit of knowing that healthcare providers are just a quick phone call away will build community confidence and comfort. Patients no longer have to drive long distances or miss work to see their doctors. There is no need to spend extra money and time on travel out of the community. Local money is kept local. With rural hospitals open more people are employed and the community is more prosperous as a whole.
- Cost savings – Telehealth is an investment with great dividends for the patients, providers, hospitals and the community. With access to broader healthcare networks, experts and resources local healthcare can improve disease management, community health initiatives, and prevent complications and hospitalizations. There is a reduced need for costly transport for strokes, heart attacks and other emergencies. Expensive hospital and emergency room visits can be quelled with home monitoring programs. Patients will save dollars in gas money, tolls and parking if they no longer have to travel to distant urban locations (not to mention lost time at work).
Telehealth in Action
Implementation of telehealth programs have demonstrated some real-world savings.
Between 2003 and 2007, the Veterans Health Administration saw a 19.7% reduction in hospital visits from 30,000 patients enrolled in a home telehealth program. The VA also saw the per-year cost for each patient drop from $13,000 to $1,600 for home-based care.
The Georgia Partnership for Telehealth which established access at 350 locations including schools and jails found emergency visits by children dropped 27% at five schools.
In North Carolina, hospitalization rates for seniors fell 25% for patients enrolled in a telehealth program over three years.
In the United Kingdom, a 2011 study found telehealth use produced:
- 20% reduction in emergency room admissions
- 15% reduction in emergency room visits
- 14% reduction in elective admissions
- 45% reduction in mortality for patients with chronic conditions
From reviewing medical records to charting healthcare plans, from reading x-rays to performing robotic surgery, from home health to specialized intensive care units, telemedicine is making healthcare more available to everyone.
Telehealth Adoption Statistics
Despite the benefits offered by implementing telehealth in rural settings, statistics provided by the RUPRI Center for Rural Health Policy Analysis culled from a 2013 HIMSS study, report that rural hospitals are lagging behind their urban counterparts stating that “rural hospitals were significantly less likely to have multiple services than were urban hospitals.” According to the report
Telehealth adoption will perhaps pick up steam in the coming years. A study by IHS states that by 2018 telehealth users worldwide are estimated to reach 7 million.
What to Look for in a Telehealth Vendor
As hospitals take on these new technologies, there are a few things few considerations to keep in mind.
For one, be sure patients can connect with a physician through video chat. Patients want to see and hear the doctor.
Also, look for systems that are simple to use with intuitive directions devoid of technical jargon and in language easy for users to understand.
There should be a chance to test-drive the system, cameras and all equipment.
Users should be able to select their own physicians and there should be a list of physicians on the system.
The physician should be able to provide a summary after the session so users can revisit instructions and advice.
Caveats
There are concerns when discussing the addition of telemedicine systems to smaller or rural critical access hospitals. Cost is the first hurdle that comes to mind. Purchase, installation and training on video-conferencing and computer systems may seem daunting but prices have gone down in recent years and costs can be negotiated. Also, there are programs available that will reimburse for set up costs.
Worries also crop up around quality and constancy of care. How do local providers maintain competency in high risk and/or low volume procedures if all patients in need are referred to the telemedicine providers? Hospitals must find creative solutions to this question, which could include rotating staff through other nearby facilities on a regular basis, better use of skill simulation labs, and using the teleconferencing capabilities of the new equipment to take part in distance education courses.
Conclusion
Telehealth is not the answer to all ills for rural hospitals in the United States. However, it can provide some much-needed options and opportunities that have not previously existed. The local hospital is often the life’s blood of the community as an employer as well as a healthcare provider. It can be the difference between life and death for many people, and finding creative means to keep them open is a challenge healthcare providers must meet.