The healthcare industry is a complex web of services, specializations, and patient needs. Referral coordinators are at the heart of this intricate system and act as the nexus between various healthcare entities. However, this critical role has challenges that can impede efficient patient care delivery. Let’s unravel the ten most common challenges referral coordinators face daily.

Photo by on Pexels
1. Inefficiency in Manual Processes
The traditional paper-based referral method is riddled with drawbacks. It’s slow, prone to human error, and often causes treatment delays. Referral coordinators are burdened with paperwork, which steals precious time that could be spent on more meaningful tasks such as patient engagement. ReferrralMD, or a referral management solution, improves efficiencies and optimizes office staff time. Work smarter, not harder.
2. A Labyrinth without a Map: Tracking Referrals
Once a referral slips into the healthcare system, tracking its progress can be akin to finding your way through a labyrinth without a map. The lack of effective tracking mechanisms makes it difficult for coordinators to monitor referral status, potentially leading to missed patient appointments and delayed treatments.
3. The Case of the Lost Referrals
Referrals can sometimes vanish into thin air within complex healthcare systems as if by sleight of hand. Miscommunication or system errors can lead to referrals not reaching their intended destination, frustrating patients and providers.
4. The Error Element: Inconsistent Data
A small typo or an incorrect patient detail can snowball into significant issues. Data inconsistencies and inaccuracies can lead to improper care, misdiagnosis, or redundant testing — thus jeopardizing patient trust and safety.
5. Who’s on First: Limited Accountability
In the convoluted referral process, who is responsible for each step can be unclear. This ambiguity can cause tasks to fall through the cracks and add to the confusion when problems must be addressed.
6. Broken Telephone: Communication Gaps
The ‘broken telephone’ game between primary care providers, specialists, and patients can lead to misinformed parties and incomplete care. Effective communication is critical, yet it remains one of the more persistent challenges in referral coordination.
7. Out of Reach: Accessibility Issues
Not all patients can access the specialists they need due to geographical or network constraints. Coordinators must navigate these barriers to connect patients with the appropriate care, often requiring innovative solutions.
8. The Compliance Conundrum
Staying compliant with ever-evolving healthcare regulations and privacy laws is a full-time job. Ensuring that referrals are managed within these guidelines is critical but can be a complex problem for coordinators.
9. Follow-Up Foibles
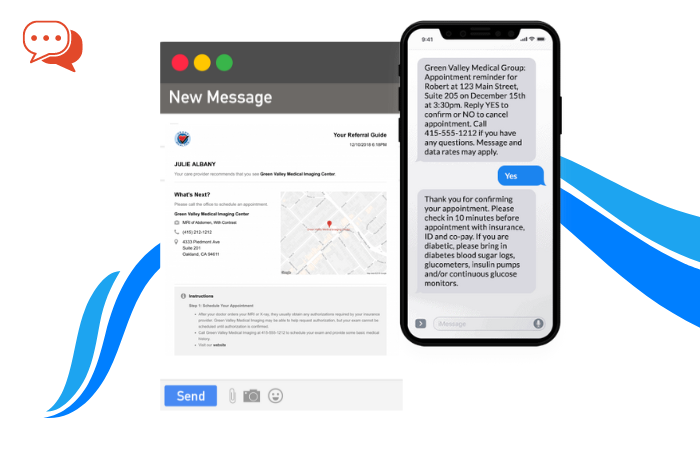
Ensuring patients follow through with their referrals is vital for continued care. However, patient follow-ups can be a significant challenge without an automated system for reminders and tracking, which may lead to dropped care plans.
10. Teething Troubles with Technology
Introducing new technologies can streamline the referral process. However, integration with existing systems can be a headache for coordinators, often leading to resistance from staff or underutilization of new tools.
Charting a Course to Solutions
Addressing these problems is no small task but critical for improving healthcare delivery. Investing in comprehensive referral management solutions that automate and streamline the process can minimize errors, ensure compliance, and improve patient satisfaction. These solutions provide a more straightforward path through the referral maze, ensuring no patient gets lost.
For the healthcare industry to evolve, it must embrace technologies and strategies that tackle these challenges head-on, empowering referral coordinators to carry out their roles with increased efficiency and confidence. Here’s to transforming the complexity of referral coordination into a journey of seamless connections and successful patient outcomes.